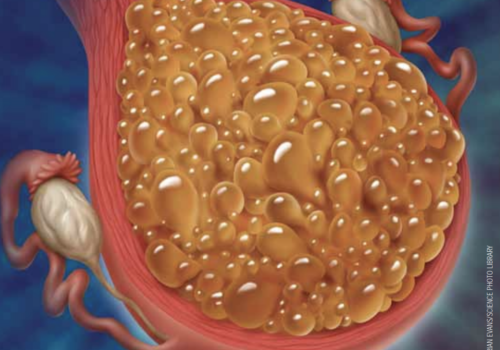
Abnormal proliferation of placental tissue inside the uterus leads to a spectrum of rare benign and malignant lesions that include molar pregnancy and together constitute gestational trophoblastic disease (GTD). GTD can be challenging to diagnose, and primary healthcare professionals should be aware of its signs and symptoms to ensure prompt and appropriate referral.