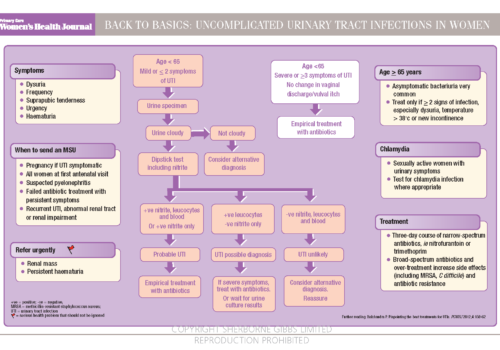
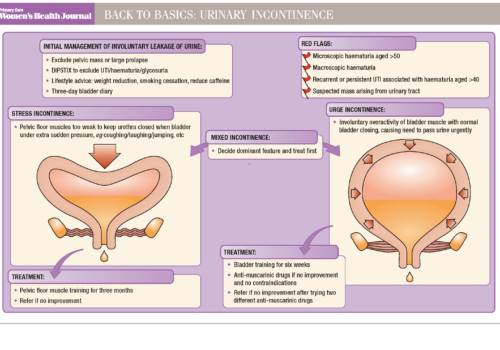
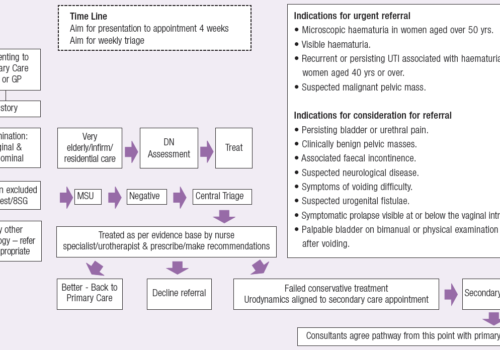
Urinary incontinence and related conditions have a high prevalence and a major impact on a patient’s quality of life. Drug therapy can be very effective and forms an important part of the treatment armoury when managing women with incontinence. Unfortunately, medication can be associated with adverse effects, but there are approaches that can be used to maximise a drug’s effectiveness and limit problems that reduce adherence to treatment.