Glycaemic index (GI) is a hot topic, often misunderstood by healthcare professionals and patients. This article fills the gaps by explaining the low-GI diet in detail, describing the benefits and barriers to using GI in practice, the benefits in patients with diabetes and the controversy that surrounds it. The aim is to help primary care professionals to make informed decisions on when and how to use GI in helping patients with diabetes to plan their diet.
Effective management of type 2 diabetes requires tight control of blood glucose levels to prevent long-term complications. Recently a number of new oral therapies have become available to help patients achieve this goal. This article provides information on how each agent works, how these different agents may be used, and the side-effects to look out for.
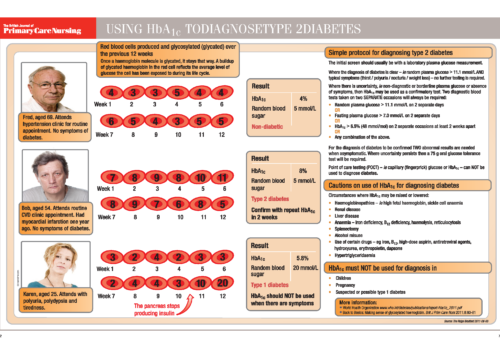
The National Institute for Health and Clinical Excellence (NICE) recommends that all people with diabetes should receive nine key tests at their annual diabetes review. These important markers ensure diabetes is well controlled and are designed to prevent longterm complications. The nine key tests are: weight, blood pressure, smoking status, HbA1c, urinary albumin, serum creatinine, cholesterol, eye examinations and foot examinations. This review discusses the importance of each marker of improved long-term care of patients.
What are the practicalities of supporting people with diabetes who fast during Ramadan? Practice nurses can make a real difference by educating patients before Ramadan starts and advising them on what they need to consider before starting their fast. Patients need to be involved in the whole process so that they are well aware of the importance of managing their diabetes to ensure good control of their glucose levels throughout Ramadan. We review how to assess patients before Ramadan, what adjustments to make to medication and how to follow up.
Fasting during Ramadan means that you have longer gaps between meals than usual. Many people also eat more food in one meal – in particular, more carbohydrate-rich and fatty foods – during this time. If you have diabetes, this may mean that you have large swings in your blood sugar levels during Ramadan. During the day – when you are fasting – your blood sugar is likely to drop. This may make you feel weak, tired and dizzy. This is called hypoglycaemia (which means low sugar) – a period of hypoglycaemia is sometimes called a ‘hypo.’ People who are sick or whose health may be adversely affected by fasting – such as those with diabetes – do not have to fast during Ramadan. However, some people do decide to observe the fast. This leaflet gives you some tips on how to keep well.
One in 20 of the UK population—or 2.8 million people—have been diagnosed with type 2 diabetes, according to a recent report based on the Quality and Outcomes Framework (QOF) exception data. Most of these patients will have been identified in primary care, and GPs and practice nurses will be only too well aware of the burden of illness associated with the cardiovascular and microvascular complications of diabetes. The most effective means of reducing the risk of these microvascular complications is to ensure that each patient achieves and maintains their individualised glycaemic target. Recent guidance from the National Institute for Health and Clinical Excellence (NICE) provides recommendations on using liraglutide (Victoza), a new option for patients who do not achieve their target HbA1c using currently available therapies.
Key issues in the management of older patients with diabetes involve both clinical skills and apatient-oriented approach. Ageing and co-morbidity may make management challenging, andclinicians need to be alert to factors such as impaired cognitive function, depression andincreased susceptibility to hypoglycaemia.
The new coalition government of the United Kingdom (UK) has announced plans to change the NHS radically in England. The Department of Health has published two important documents Equity and excellence: liberating the NHS and Liberating the NHS: commissioning for patients. The implications for primary and secondary care, and for local authorities, mental health services and community providers, will be enormous. The changes are taking place at a rapid pace and every manager and clinician in the NHS will need to keep abreast of developments as they will affect the way in which we all deliver services in the future.
Today, many people with type 2 diabetes who need insulin have their insulin initiated in primary care. Here we discuss NICE recommendations for initiation and management of insulin, and the different types of insulin and delivery systems.
The most effective means of reducing the risk of complications associated with type 2 diabetes is to ensure that each patient achieves and maintains their individualised glycaemic target. New guidance from the National Institute for Health and Clinical Excellence (NICE) providesrecommendations on using liraglutide (Victoza), a new option for patients who do not achieve target HbA1c using currently available therapies.
A unique new e-platform for primary care

For healthcare professionals in countries with applicable health authority product registrations. The content may not be approved for use in your specific region or country. Please review the applicable product labelling for your country for indications and instructions prior to use. If not approved, please exit this site.
We use cookies to ensure that we give you the best experience on our website.
By continuing to this site you are confirming that you are a healthcare professional and are opting into the use of cookies.



















