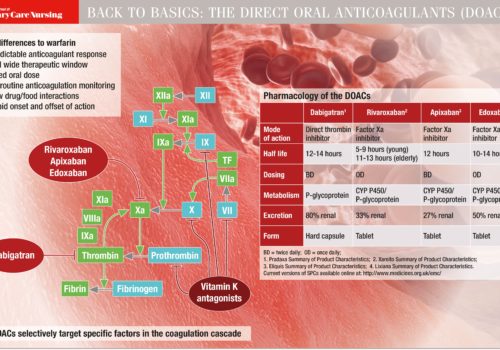
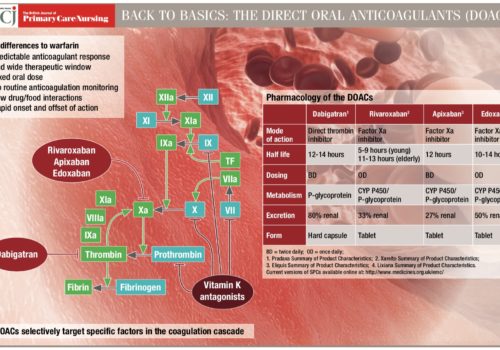
Atrial fibrillation (AF) management has been transformed within the last decade by revised clinical guidance and availability of new drugs. Aspirin monotherapy, once accounting for almost half of all antithrombotic prescriptions for AF, is now an obsolete therapy. Anticoagulation is the treatment of choice for AF and direct oral anticoagulants (DOACs) have overtaken warfarin as the drug of first choice for new starters. However, management of one in four people with AF remains suboptimal, and this article reviews the major issues around antithrombotic and other treatments for AF.