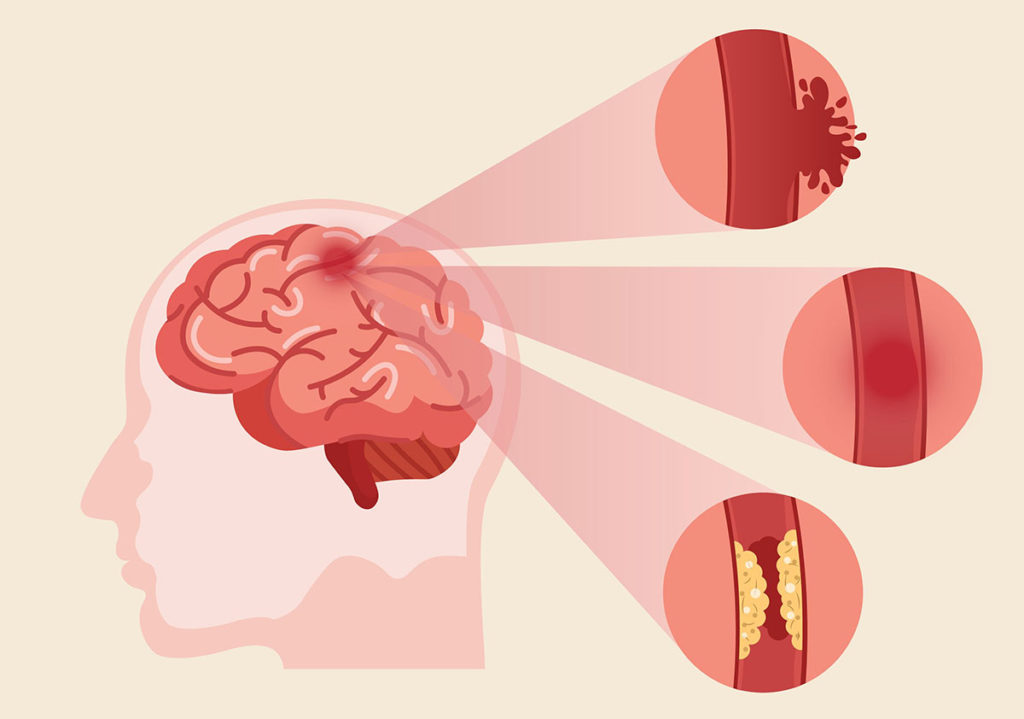
Transient ischaemic attack (TIA) is an important risk factor for stroke. Early recognition of symptoms and timely secondary prevention significantly reduce stroke risk. We review current evidence and guidelines for early management and treatment of TIA, including early antiplatelet therapy, specialist review, and recognition and treatment of other risk factors. The roles of carotid artery and brain imaging are also considered.