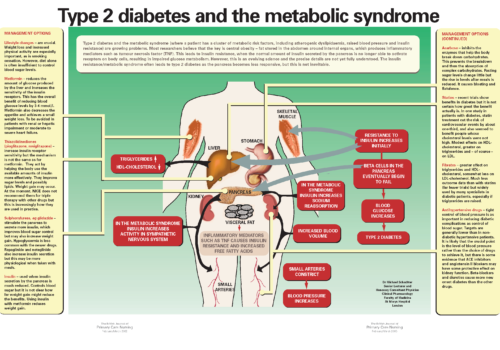
The metabolic syndrome is a bit like smoothie makers. Everyone’s heard of them, many people seem to have them, but no-one is quite sure what to do with them. So let’s have a look at how the metabolic syndrome came to enter our vocabulary, what it really means and whether it is something that could help us to look after our patients better or just another cumbersome tool that produces a lot of heat but no light.