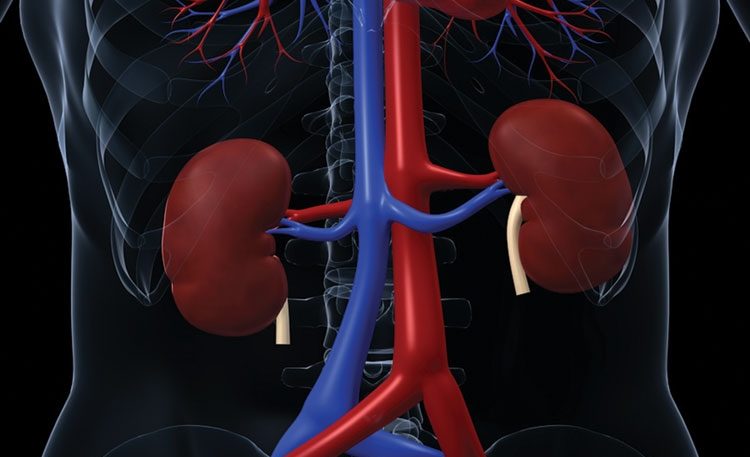
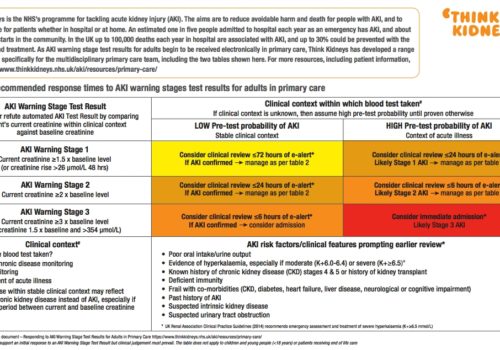
Heart failure (HF) is a devastating clinical syndrome characterised by a constellation of symptoms and signs in the presence of reduced cardiac function. Comorbidity is almost inherent as HF is often the culmination of chronic disease processes such as ischaemic heart disease, hypertension and valve disease and its treatment may precipitate comorbidities such as gout, erectile dysfunction (ED) and acute kidney injury (AKI).