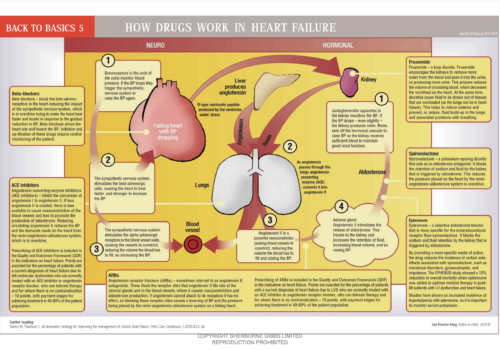
Heart rate appears to be a marker for optimal medical therapy in heart failure, and a key determinant of hospitalisation. This study compared practices using the local enhanced service (LES) for heart failure against those not delivering the LES. Education and heart rate control seem to influence hospitalisation rates.