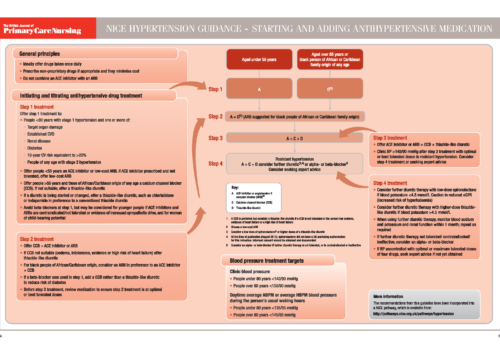
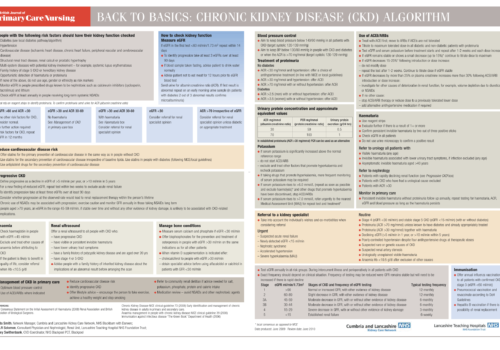
Peripheral arterial disease (PAD) forms part of the same generalised vascular disease as coronary heart disease and cerebrovascular disease. Recent National Institute for Health and Clinical Excellence (NICE) guidelines emphasise the importance of a standardised approach in primary care. The aims of this article are to provide an update for practice nurses, and to highlight the importance of asymptomatic PAD as an independent risk factor for cardiovascular morbidity and mortality.