What a winter we have had! Many children have seen heavy snow fall for the
first time and London was completely immobilised due to the weather. At the
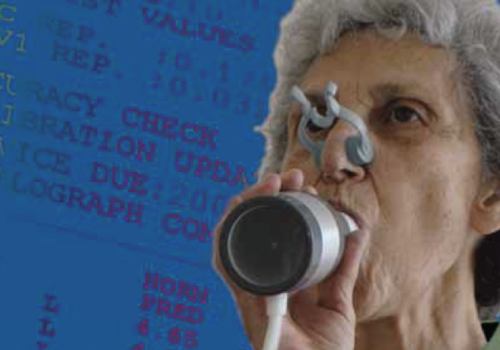
same time our hospitals have been battling to cope with patients suffering with
respiratory infections and exacerbations of their COPD. GP practices have been
stretched to the limit to cope with the additional burden of coughs and colds.
Building capacity is a real problem for everyone working in the health service and
patients’ demands and expectations continue to grow.



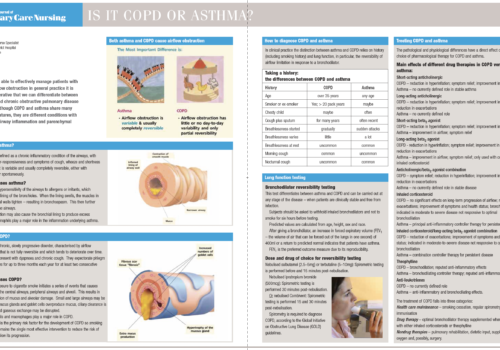
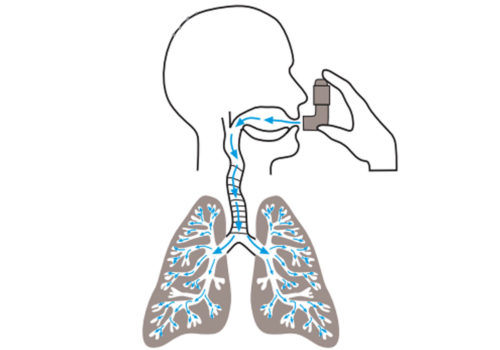
 About chronic obstructive pulmonary disease.
About chronic obstructive pulmonary disease.