There are several different drug types used in the management of hypertension. This back to basics provides a useful summary of the different antihypertensive drug classes and how they act to regulate blood pressure.



View Chronic obstructive pulmonary disease (COPD) Articles
 About chronic obstructive pulmonary disease.
About chronic obstructive pulmonary disease.
Chronic obstructive pulmonary disease (COPD) affects about 1.2 million people in the UK making it the second most commonly diagnosed respiratory disease. The number of patients with COPD has been steadily increasing and the predominantly older (>60 years) patients often present with varying degrees of emphysema and chroninc bronchitis.
Diagnosis of COPD generally requires spirometry and a chest x-ray and blood counts to exclude anaemia and polycythaemia as well as calculations of body mass index (BMI) and oxygen saturation.
A critically important first step in the management of COPD is smoking cessation, where appropriate.
Other common interventions include pneumococcal and annual influenza vaccinations and dietary intervention to promote weight loss.
Inhaled corticosteroids, long acting muscarinic antagonists and long acting beta agonists (LABAs) are the foundation of therapy for Chronic obstructive pulmonary disease – underling the importance of educating patient to use their inhalers appropriately.

People with COPD should be reviewed at least annually according to the Quality and Outcomes Framework. However, there is little mention of the importance of assessing nutritional status and no ‘QOF’ points for doing so. This article describes the assessment and management of COPD patients with a risk of malnutrition.

Chronic obstructive pulmonary disease (COPD) is a largely preventable, slowly progressive, inflammatory disease. Rates of COPD are rising faster in women than in men, yet women are less likely to be diagnosed. There is currently no cure, but best-practice management outlined in recently updated NICE guidelines can help to improve patients’ symptoms and quality of life.

Chronic clinical conditions have traditionally been regarded as individual disease categories within individual patients, although there is often considerable overlap across clinical systems. However, for those managing these patients the presence of various co-morbidities is all-too apparent. It may be time to consider a new approach to management of these patients.
Cardiovascular morbidity and mortality in patients with chronic obstructive pulmonary disease (COPD) is nearly double the rate in the general population without COPD. And for those with cardiovascular disease (CVD) and COPD, heart failure is the most common cause of hospitalisation.

Chronic obstructive pulmonary disease (COPD) is the term used to describe a range of
chronic chest conditions, including chronic bronchitis and emphysema. COPD is
characterised by permanent damage to the lungs and as the condition develops, people
experience increasing breathlessness, to the point where even everyday activities such
as getting dressed or walking up stairs become difficult. This article describes the impact of
COPD, explores the value of exercise in COPD management and discusses possible reasons for its
widespread under-use as effective symptom control.

What a winter we have had! Many children have seen heavy snow fall for the
first time and London was completely immobilised due to the weather. At the
same time our hospitals have been battling to cope with patients suffering with
respiratory infections and exacerbations of their COPD. GP practices have been
stretched to the limit to cope with the additional burden of coughs and colds.
Building capacity is a real problem for everyone working in the health service and
patients’ demands and expectations continue to grow.
Diagnosing chronic obstructive pulmonary disease (COPD) can be complex and requires
considerable clinical skill. It is rather like putting together the pieces of a jigsaw
puzzle. But don’t despair. In this article, we take you through the key steps. A careful
history, particularly in smokers or ex-smokers who complain of breathlessness,
followed by clinical examination may indicate possible COPD. Further steps must then be taken
to exclude other causes of respiratory symptoms and spirometry is essential in diagnosing
airflow obstruction, which may help to confirm the diagnosis of COPD.
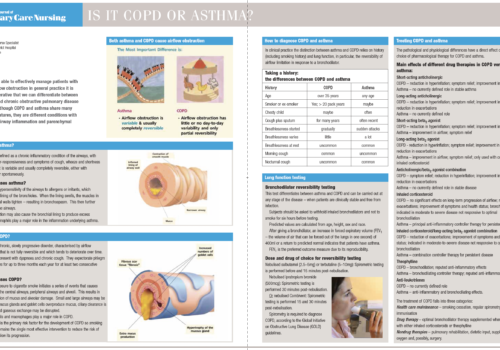
To be able to effectively manage patients with
airflow obstruction in general practice it is
imperative that we can differentiate between
asthma and chronic obstructive pulmonary disease
(COPD). Although COPD and asthma share many
clinical features, they are different conditions with
different airway inflammation and parenchymal
patterns.
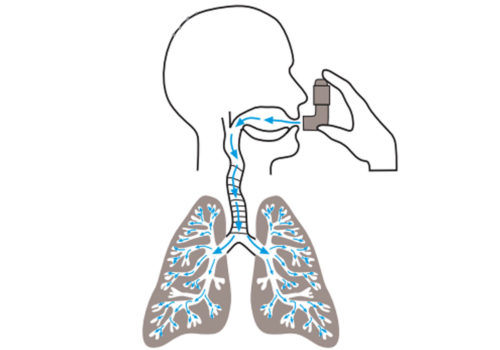
Asthma UK estimates that 2.1 million patients in the UK are suffering unnecessarily because
they do not use their asthma treatment effectively. This article looks at how inhaled
therapies are deposited in the lungs, and at the basic differences between inhalers – with
a focus on optimising inhaler technique.
A unique new e-platform for primary care

For healthcare professionals in countries with applicable health authority product registrations. The content may not be approved for use in your specific region or country. Please review the applicable product labelling for your country for indications and instructions prior to use. If not approved, please exit this site.
We use cookies to ensure that we give you the best experience on our website.
By continuing to this site you are confirming that you are a healthcare professional and are opting into the use of cookies.


















