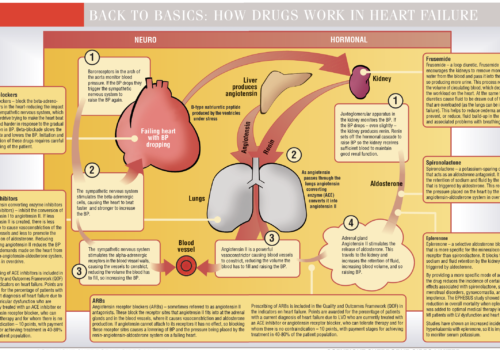
Heart failure (HF) is an important cause of morbidity, mortality and misery for patients. However, there are many ways to improve and extend the lives of people with HF, if clinicians are familiar with and apply the numerous traditional, less mainstream and more innovative evidence-based treatment options. This article reviews current best practice in the management of chronic HF and of acute decompensated HF, and considers recent insights, controversies and innovations in this important, fast moving field.