It looks like it is going to be a long hard winter. The media have already been reporting restrictions on referrals and rising waiting times. It is likely that things can only get worse given the pressures on primary care trusts and local authorities. At times of economic stringency, women’s sexual and reproductive health can seem an easy target. But this is short-sighted and probably not costeffective given the UK’s high rates of teenage pregnancy and sexually transmitted infections. It is time for an approach to service configuration that goes beyond knee-jerk slash and burn.
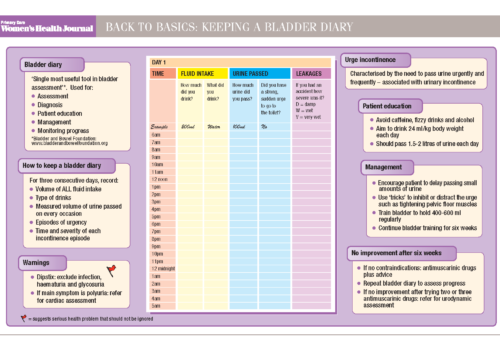
Back to Basics: Keeping a Bladder Diary
Chlamydia in women
Challenging the rule of halves in osteoporosis
Half of post-menopausal women will suffer a fracture during their lifetime, mainly because of osteoporosis. Currently available medication can halve the risk of future osteoporotic fractures. Yet many at-risk women are still unidentified, and only half of all patients persist with treatment for more than a year.
Viewpoint
Twenty-five years ago, few healthcare professionals associated osteoporosis with an increased risk of broken bones, and there was no internationally recognised definition of the disease. There were no NHS dual X-ray absorptiometry scanners, treatment options were limited, and the care and support offered to those with osteoporosis was a long way below the standards delivered by health professionals today. There was also no UK-wide charity to raise awareness of the disease.
Pass it on: the reality of inherited cancer risk
Many people have close relatives with cancer, and the possibility of inherited risk is increasingly raised during a GP consultation, often by patients themselves. It is important to identify the small but significant proportion of people who are at greatly increased risk of developing cancer as a result of their family history. But most patients with a family history are not at higher risk, and can be managed in primary care.
Put out the fire of vulvodynia
Most often described as a burning pain, vulvodynia is a chronic pain syndrome that affects all or part of the vulva. Diagnosis of this distressing condition is frequently delayed and management is challenging. But careful diagnosis and appropriate referral can help to minimise pain and enable women to regain control of their lives.
Taking control of urinary continence in women
Urinary continence problems are common in women, and result in significant costs to patients, carers and the NHS, both for treatment and coping strategies such as pads and appliances. Despite this, continence rarely gets the attention that some other, less prevalent conditions receive, and there is evidence of both under-diagnosis and inadequate management.
Age no barrier: Contraception in the perimenopause
Although there is a natural fall in fertility with age, women still need reliable contraception to avoid unintended pregnancies during the perimenopause. No contraceptive method is contraindicated by age alone, but women must be individually assessed, based on the risks and benefits of each method.
Towards the rational prescribing of oral contraceptives
This supplement is supported by Consilient Health Ltd on behalf of whom this Expert Working Group was convened and funded. Consilient Health Ltd also provided a framework for the discussion.
Effective prescribing of the contraceptive implant
This supplement was developed in conjunction with and its production paid for by Merck Sharp & Dohme Limited.
Editorial
The Department of Health certainly gave us all something to think about over the Christmas break and well into the New Year. In the middle of last December, Secretary of State Andrew Lansley confirmed that the Coalition Government is pressing ahead with its radical structural changes to the NHS in England.1 This was despite concerns by professional and patient organisations, and indeed the House of Commons Select Committee,2 about the feasibility of introducing major reforms when the NHS is under increasing financial pressures.