Genital herpes is a common sexually transmitted infection, especially among young adults. It may be associated with complications, notably in pregnant women, but it is not usually life-threatening. However, the diagnosis continues to attract stigma, and patients need reassurance and support as well as effective treatment.
Connecting for Women’s Healthcare
One of the great by-products emerging from the Primary Care Women’s Health Forum (PCWHF) is connectivity. Our members are becoming more aware of local initiatives in other parts of the country, and are connecting with and learning from other clinicians to share best practice in women’s healthcare.
Take a new approach to premenstrual disorders
Premenstrual disorders (PMD) are common and have a major impact on the lives of women. Until recently there has been confusion around definitions, leading to difficulties in diagnosis and management. This article describes a new consensus definition and diagnostic criteria for PMD, and advises on the choice of evidence-based treatment.
Made to measure: Tailoring oral contraception to each woman
Individualising choice of oral contraception to each woman is important to ensure safety, and enhance patient acceptability and adherence. However, tailoring should extend beyond simply deciding whether to use a combined or progestogen-only pill. Prescribers should also bear in mind the non-contraceptive benefits of each product, and consider alternative regimens for women with hormone-related medical conditions or those who wish to avoid menstrual bleeds.
Fertility problems
If you have fertility problems, it means you have difficulty in conceiving (becoming pregnant) despite having regular sex without using contraception. Before you begin to worry, remember that many couples take several months to conceive. Over eight in 10 couples conceive within a year of trying, while about nine in 10 conceive within two years.
Practical prescribing to promote urinary continence
Urinary incontinence and related conditions have a high prevalence and a major impact on a patient’s quality of life. Drug therapy can be very effective and forms an important part of the treatment armoury when managing women with incontinence. Unfortunately, medication can be associated with adverse effects, but there are approaches that can be used to maximise a drug’s effectiveness and limit problems that reduce adherence to treatment.
Editorial
For over two years now, I have been worrying that my editorial will be out of date by the time you read it because the Department of Health has published its sexual health policy document. At the time of writing, the document has yet to appear (though the Department’s website still reassures us it is due to be published in 2012). So local authorities may be taking over responsibility for contraception and sexual health in a public health policy vacuum. If this is the case, it can only compound current variations in provision, especially of long-acting reversible contraception (LARC).
Guest editorial
Teenage conceptions continue to raise interest in the media, with young people often demonised about their early or allegedly frequent sexual activity. When conception rates are published, commentators waste no time in telling us how dreadful the situation is and how we compare with other Western European countries. Of course, we are not like our neighbours in Europe, as we do not have mandatory sex education for all young people, and we live in a highly sexualised society where sex is often the material for jokes.
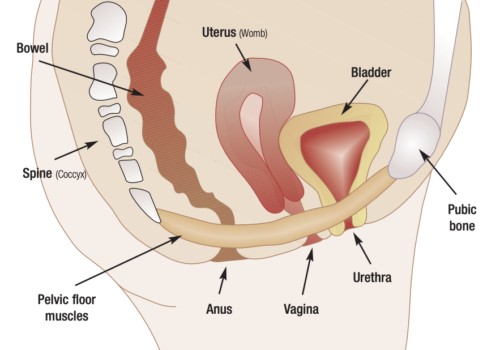
Teach pelvic floor muscle exercises
Over the past 30 years a wealth of research has proved the benefits of pelvic floor muscle exercises (PFME) in treating both urinary incontinence and pelvic organ prolapse. However, patients in some areas may have to wait some time for an appointment with specialist continence services. So it makes sense for primary care professionals to know how to teach PFME to their patients.
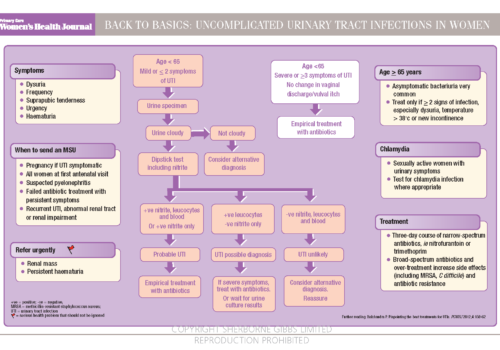
Back to Basics: Uncomplicated urinary tract infections in women
Born still, but still born: Understanding stillbirth
After the second trimester, it is generally assumed that a pregnancy will end with the joy of a newborn baby. But the reality is that each year in the UK, one in every 200 – or around 4,000 – babies die in the third trimester before, or during, labour. This is one of the highest rates of stillbirth among high-income countries, and each death has profound effects on the woman, her family and health services.
Contraceptive choices for women with diabetes
Unplanned pregnancy with poor glycaemic control at conception is associated with major maternal and perinatal complications. However, contraception is used haphazardly by women with diabetes and is often not discussed by diabetes professionals. GPs and practice nurses need to be able to give appropriate advice about contraception to the increasing numbers of women of childbearing age with type 1 and type 2 diabetes.