Heart failure (HF) is a complex clinical syndrome, characterised by symptoms including breathlessness, fatigue, reduced exercise tolerance and fluid retention. Signs and symptoms may be non-specific or difficult to elicit, and some primary healthcare professionals continue to lack confidence in their ability to identify patients with HF. A systematic approach to history-taking, examination and referral aims to help improve the accuracy of the diagnosis and ensure that HF patients are referred for specialist assessment and receive evidence-based therapies.
How many more people will we need to anticoagulate using CHA2DS2VASc? A real-life study in British primary care
Managing stroke risk in people with atrial fibrillation (AF) is critical. The introduction of the CHAVASc score has lowered the threshold for consideration of anticoagulation to prevent stroke in AF. This means potentially extra work for clinicians in assessing AF patients, and an extra cost to the NHS from more medication and monitoring. This study aims to quantify the increase in the numbers of people requiring anticoagulation with the newer risk assessment score. Method: The GRASP-AF tool was used to quantify the number of people categorised as high risk, using the CHAVASc score compared with the standard CHADS score. Population: An inner-city population from nine general practices within a single Clinical Commissioning Group (CCG), covering a population of 42,274 patients. Results: A total of 395 patients were found to have AF. In this study, 64% were categorised as high risk using CHADS compared with 87% on CHAVASc. This represents an increase of 35% in the numbers of people classed at high risk of stroke and needing to be considered for anticoagulation. Conclusion: There are significant extra costs to implementing the CHAVASc score, both in drug costs and extra work for primary care, which need to be managed within the local health system. The greatest benefit will be at an individual level. Some people who would have had a stroke will be spared that experience. Who those individuals are, we will never know.
Living with frailty: A guide for primary care
Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their in-built reserves. This means the person is vulnerable to dramatic, sudden changes in health triggered by seemingly small events such as a minor infection or a change in medication. BJPCN, Volume 12, Special Issue 1, Jan-Feb-Mar […]
Updated NICE CKD guidelines: What they mean for your practice
Since the publication in 2008 of the first NICE guideline on the diagnosis and management of chronic kidney disease (CKD), there has been concern that creatinine-based estimated glomerular filtration rate (eGFR) may not accurately identify people at increased risk–particularly in elderly populations. The updated NICE guideline, issued in July 2014, includes some important changes that take into account recent research into the prognosis of CKD. Of particular relevance for GPs are changes to the diagnostic criteria and classification of CKD, which are described in this article.
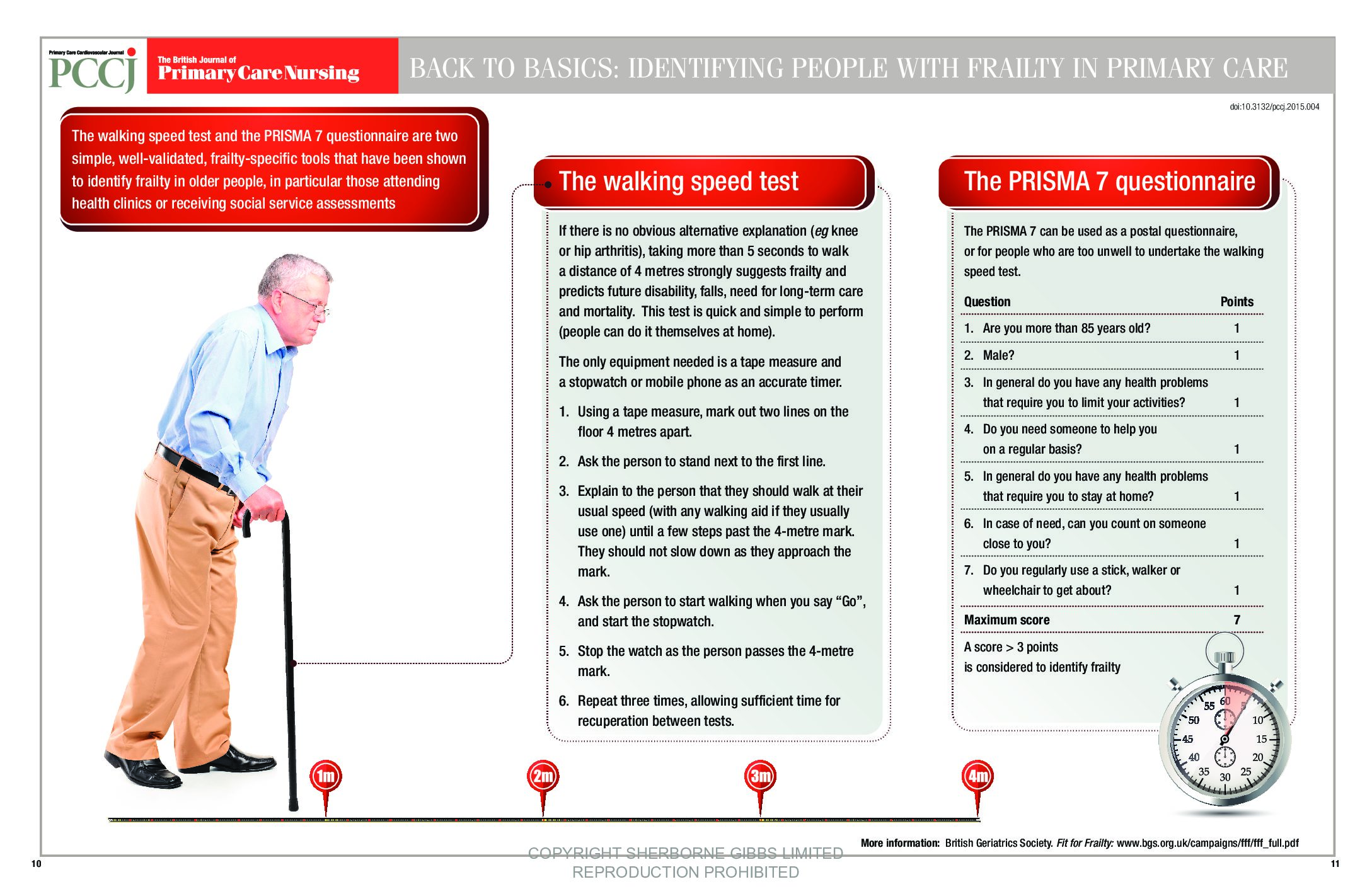
Back to Basics: Identifying people with frailty in primary care
Why we need a new approach to managing people with frailty
Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their in-built reserves. This means the person is vulnerable to dramatic, sudden changes in health triggered by seemingly small events such as a minor infection or a change in medication.
Understanding frailty as a long-term condition
Acommonly heard clinical expression is “He/she is very frail”. It provides a summary statement of an older person that implies concerns over vulnerability and prognosis. This is how we have conventionally considered frailty—as a descriptive label: ‘the frail elderly’. In this article, we will re-frame frailty in a potentially more helpful way. We will examine frailty from the perspective of an abnormal health state that behaves just like a long-term condition. This conceptualisation of frailty opens up new approaches to helping people who are frail.
Improving end-of-life care in the community
Most nurses are involved in the care of the 1% of the population currently nearing the end of their lives: that is, people considered to be in their final year, months, weeks or days of life. The Gold Standards Framework (GSF) programmes can help provide a structured framework in this challenging area, leading to more proactive and consistent standards of care, and enabling more people to live well and die well where they choose.
Care and support planning for people with frailty
Supported self-management is feasible and desirable for people with mild frailty, but care and support planning is more appropriate for individuals with moderate frailty. This section considers how the primary healthcare team can apply a whole person and personalised approach to care and support planning.
Supported self-management for people with frailty
The first section of this supplement made the case to consider frailty from the perspective of a long-term condition. This and the next section explore what this means in terms of applying some of the well-developed models for the care of longterm conditions to people who are living with frailty. First, we examine how the highly evidence-based model of supported self-management might be applied to frailty.
Blood pressure: A call to action for primary care
Over the next 10 years, an estimated 45,000 quality-adjusted life-years and £850m health and social care costs could be saved, if England saw a 5 mmHg reduction in the average population systolic blood pressure. In addition, substantial reductions in death and disability could be achieved if there was a step change in our approach to detection and treatment of hypertension. This is the rationale behind the Blood Pressure Action Plan that was published recently.
Ensuring the safe use of insulin in diabetes
Insulin therapy is life-saving for people with type 1 diabetes, and a key component of the treatment regimen for many people with type 2 diabetes. At the same time, insulin is a major cause of adverse drug events, some of which are so severe that they cause emergency admission to hospital. There is therefore much that needs to be done to improve the safe use of insulin in order to reduce medication errors and hospitalisation associated with hypoglycaemia.