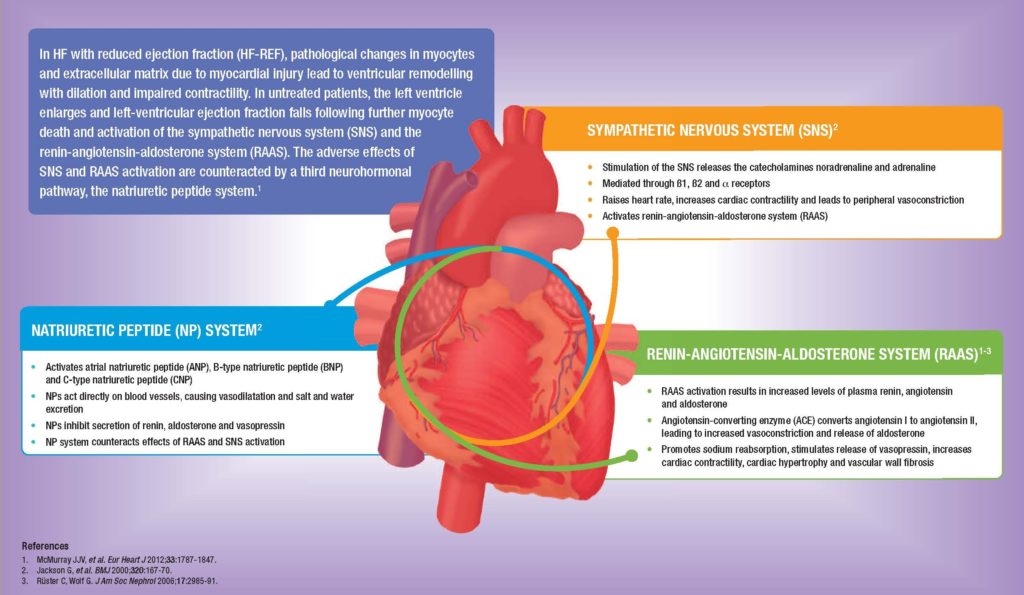
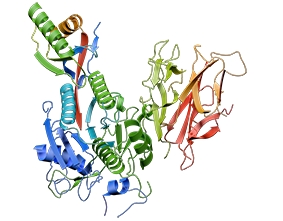
This useful Back to Basics poster describes the damaging changes that take place in three key body systems when HF with reduced ejection fraction is left untreated. The sympathetic nervous system, the renin-angiotensin-aldosterone system and the natriuretic peptide system all undergo significant pathophysiological changes as HF progresses.
Heart failure in the UK: We can do better
The UK faces an epidemic of heart failure (HF). NICE guidelines emphasise the importance of multidisciplinary assessment and care by HF specialists, evidence-based prescribing, and careful discharge planning after hospitalisation. This article highlights areas where improvements can be made in the management of HF including taking lessons from the latest National Heart Failure Audit.
Sacubitril/valsartan in heart failure: A guide for primary care
This issue introduces a first-in-class oral treatment for heart failure – sacubitril/valsartan. It provides a comprehensive background to heart failure treatment in the UK, the pathophysiology of the disease and the pivotal trial data on the new drug. Articles give perspectives on the role of the GP, practice nurse, pharmacist and commissioner in using the […]
New international survey highlights education needs in cholesterol management
The European Atherosclerosis Society has conducted a survey to assess the general public’s understanding of cholesterol. Professor Mike Kirby summarizes the survey findings and highlights the importance of a clear and constant focus on the JBS3 2014 consensus recommendations.
PCSK9 inhibition in lipid management
Two injectable antibody-based therapies inhibiting the activity of PCSK9 – alirocumab and evolucumab – have recently been licensed. This paper reviews the current status of lipid management, the actions of PCSK9, and the clinical trial results achieved with PCSK9 inhibitors in early studies.
Seasonal variation of HbA1c in diabetes
The time of year is one of a number of factors shown to affect HbA1c levels. This study investigated seasonal variations in HbA1c in a large population of people with diabetes in Scotland. These variations appear to have clinical significance in terms of making medication decisions and other aspects of clinical care.
The ‘Year of Care’ in Leeds: Implications for our practice
The ‘Year of Care’ is a systematic approach to managing long-term conditions, focused on personalised care planning where patients work with the clinician to agree goals, identify support needs, develop and implement action plans, and monitor progress. This article reports the learning from implementing ‘Year of Care’ in primary care practices in Leeds.
The five key jobs for general practice after a myocardial infarction
The updated NICE guideline on post-myocardial infarction care (CG 172) provides a benchmark for primary care. In this article, Ivan Benett and Jennifer Yung highlight the five key tasks for general practice in caring for someone who has suffered a heart attack.
AF a stronger CV risk factor for women
PCCJ Editor-in-Chief Mike Kirby reviews a recent large observational study in the BMJ which concludes that women with atrial fibrillation are at a higher risk of cardiovascular disease and death than men.
Gender and quality of life in COPD: A systematic review
Morbidity and mortality for women with COPD is increasing. This systematic review uncovers how women seem to experience COPD differently to men, and helps health care professionals to provide an individualised approach to caring for these patients.
Updated NICE guideline of type 2 diabetes management in adults
Professor Mike Kirby highlights the key updates in the new NICE guidelines on the management of type 2 diabetes in adults and how these impact your practice. The updated guideline focuses on an individualised approach to patient care with recommendations on patient education, dietary advice, managing cardiovascular risk, managing blood glucose levels, and identifying and managing long-term complications.
An innovative strategy for the management of chronic heart failure
A large amount of evidence points to the effectiveness of optimising primary care heart failure management in reducing referral to hospital and improving outcomes for patients. This article describes the changes made in a primary care practice that has resulted in measurable difference for the primary care team and their patients.