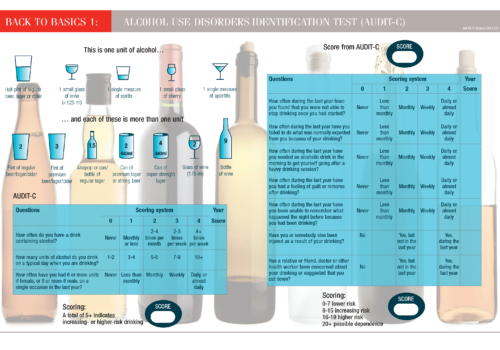
NHS Health Checks now include AUDIT-C, a brief screening tool designed to help identify people who may be problem drinkers. Taking the test can be a sobering experience for patients, but now is the time to get a grip on our national relationship with alcohol.
Ask, ask, ask…about alcohol
Back to Basics: Alcohol use disorders identification test (Audit-C)
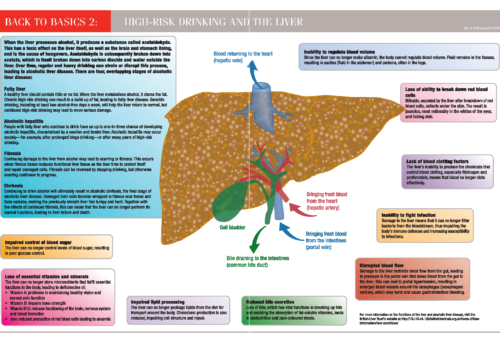
Back to Basics: High-risk drinking and the liver
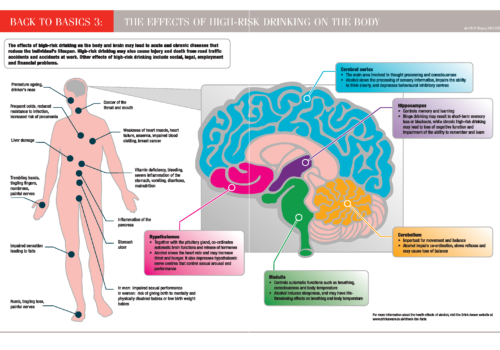
Back to Basics: The effects of high risk drinking on the body
Alcohol and the heart: food, medicine or poison?
People have been producing alcohol for thousands of years and consuming it as part of their diet as well as for medicinal purposes. When taken in moderation, drinking alcohol can be a safe and pleasurable activity with potential heart health benefits. However, those cardiovascular benefits are lost when alcohol is consumed in excess, and drinking becomes harmful with adverse physical, psychological and social consequences.
Alcohol and sex: a risky mixture for sexual health
Alcohol-related harm is a major public health concern, and since April 2013 questions to identify problem drinkers have been included in the NHS Health Check for people aged 40-74 years. But young people are also a key at-risk group for hazardous consumption, and the physical harms of alcohol may be compounded by risks to their sexual health.
Over the limit? A healthier approach to alcohol
Alcohol forms part of the diet for over 90% of adults in the UK and is unusual in being both a nutrient and a drug. For many of us, alcohol is a safe and pleasurable part of the diet. However, there is growing concern that many people who see themselves as social drinkers are consuming levels that may cause harm. Understanding how to assess safe levels of alcohol consumption and identify strategies for cutting down can help us to advise our patients how to moderate their intake.
EDITORIAL | Moving with the times
Delivering CVD care: GPs under pressure and disempowered – a qualitative study
GPs, practice nurses and other primary healthcare professionals are now at the frontline of managing cardiovascular disease (CVD) and delivering preventive care. The aim of this study was to explore clinicians’ experiences and their views on the factors that influence their ability to fulfilthis demanding role. GPs and other primary healthcare professionals expressed similar views. In particular, they reported a sense of pressure and disempowerment, and voiced concerns about the ability of general practice to take on its greater role in reducing the burden of CVD.
It’s not just a high cholesterol level, it can be an indicator of genetic disorder
7.5 mmol/L) should prompt clinicians to think of familial hypercholesterolaemia. A family history of premature heart disease should further raise suspicion. This dominantly inherited genetic abnormality deserves as much attention as the oncogenes such as BRAC 1 and 2. HEART UK – The Cholesterol Charity – has provided editorial support and review of this sponsored FH series.This article was made possible by an unrestricted educational grant by Sanofi, who had no control over content.
Chronic kidney disease, cardiovascular risk and primary care
This article describes the interrelationship between chronic kidney disease (CKD) and cardiovascular disease and defines the basis for the various interventions which have been recommended in national guidelines. It also provides a critique of currently available guidelines and suggests where changes may be desirable in future.