Nobody likes to talk about failure. We hide from it, shy away from it. Society demands positivity. And so, we do not necessarily take the time or put the effort into learning from failure. Heart Failure is a misunderstood and misdiagnosed condition, as malignant as some of the most common cancers, it should be treated with […]
Case study: The hypertensive patient
Working with patients who are not willing to engage fully with healthcare services is a common occurrence. The process requires patience and a focus on providing the patient with full information about their condition and then allowing them to make decisions about their treatment. Here, Dr Terry McCormack (GP and Cardiovascular Lead, North Yorks) describes the approach of his practice to a man with hypertension.
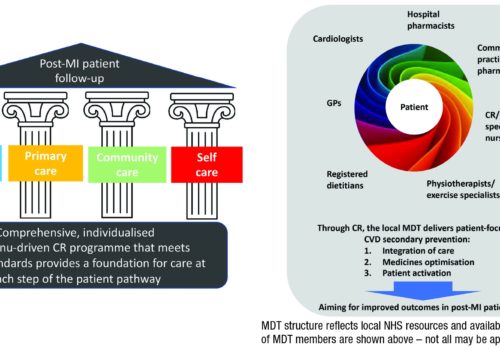
A UK consensus on optimising CVD secondary prevention care: Perspectives from multidisciplinary team members
Although overall CV mortality has declined in recent years, patients with clinically manifest CVD remain at increased risk of recurrent CV events. A group of HCPs at UK primary and secondary care centres have recently developed a consensus statement to improve delivery of secondary prevention in the UK.
Practical tools for CVD prevention: The CVD return on investment tool
In 2017 the University of Sheffield was commissioned by Public Health England (PHE) to develop a new return on investment (ROI) tool for cardiovascular disease (CVD) prevention, to be used by national and local decision-makers. The tool focuses on prevention of CVD in six key high-risk groups, identified through the NHS RightCare pathway as being currently underdiagnosed and insufficiently well managed. This includes patients with hypertension, diabetes (type 1 and type 2), non-diabetic hyperglycaemia, atrial fibrillation, chronic kidney disease and high cholesterol (the latter including patients with a QRISK2 score ≥ 10% or familial hypercholesterolaemia).
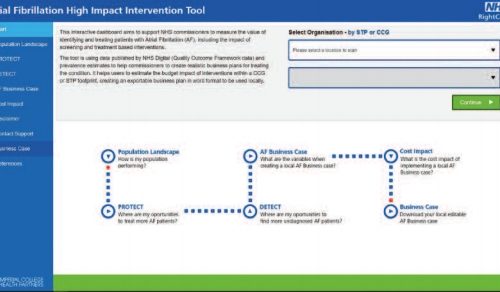
Practical tools for CVD prevention: The NHS RightCare AF high impact intervention tool
Cardiovascular disease (CVD) prevention has been highlighted by the Next Steps on the Five Year Forward View as a key priority for clinical commissioning groups (CCGs). An important area of focus is improving the management of high-risk conditions for CVD, such as atrial fibrillation (AF). In response to this escalating healthcare priority, Imperial College Health Partners have developed the new AF High Impact Intervention Tool in collaboration with NHS RightCare, as part of their CVD Prevention Pathway.
Practical tools for CVD prevention: NHS RightCare toolkit for CVD and serious mental illness
We know that there are differences in outcomes between populations that cannot be explained by the dictates of evidence-based medicine or by demographics. Core to the work of NHS RightCare is the concept of unwarranted variation and the vital importance of using our shared NHS resources to deliver the best outcomes for our population. In 2018, NHS RightCare developed the toolkit for physical ill health and cardiovascular disease (CVD) prevention in people with severe mental illness (SMI), in close collaboration with Public Health England (PHE).
Practical tools for CVD prevention: FH implementation guidance
Familial hypercholesterolaemia (FH) is a common monogenetic condition that causes high levels of cholesterol in the blood, resulting in an increased risk of heart disease at an early age. FH affects around one in every 270 people. That means that in England around 160,000 adults and 40,000 children under 18 years are likely to have FH, though only around 3,000 have been diagnosed by DNA testing. This article discusses the new implementation guide, which is designed to improve the identification and treatment of people with FH.
The Heart Age Test: An evidence-based, individual risk calculator
Behavioural risk factors such as poor diet, smoking and low physical activity, along with high blood pressure, high body mass index and high cholesterol are the main risk factors for cardiovascular disease (CVD). The Heart Age Test is a digital online tool designed to help make sense of an individual’s risk of CVD, the implications of that risk and the behavioural changes needed to reduce that risk.
Lipid lowering: Working with patients to take their tablets
The benefits of lipid modification therapy in reducing cardiovascular disease (CVD) risk have been well recognised since the advent of effective treatments, including the HMG-CoA reductase inhibitors (statins). Use of statins is likely to have been a contributory factor in the fall of over 75% in CVD mortality in many industrialised countries over the last 40 years. Other interventions, including improved management of other cardiovascular risk factors, notably hypertension and smoking, have also been important. However, CVD continues to be responsible for one in four premature deaths in the UK, with rates in the most deprived 10% of the population being almost twice as high as in least deprived cohorts.
Atrial fibrillation management: We can do better
Atrial fibrillation (AF) management has been transformed within the last decade by revised clinical guidance and availability of new drugs. Aspirin monotherapy, once accounting for almost half of all antithrombotic prescriptions for AF, is now an obsolete therapy. Anticoagulation is the treatment of choice for AF and direct oral anticoagulants (DOACs) have overtaken warfarin as the drug of first choice for new starters. However, management of one in four people with AF remains suboptimal, and this article reviews the major issues around antithrombotic and other treatments for AF.
Detect, protect, perfect: AHSNs going further, faster to reduce AF-related stroke
Since 2014 the 15 Academic Health Science Networks (AHSNs) across England have been working on a collaborative atrial fibrillation (AF) programme focused on reducing AF-related stroke. The national programme has three elements: Detect: finding more people with AF to allow early intervention to prevent stroke; Protect: treating more at-risk patients with anticoagulants to reduce the rate of AF-related stroke; and Perfect: improving the quality of anticoagulation to ensure maximal patient outcomes.
Pharmacist-led interventions for CVD prevention
Community pharmacists are widely recognised as an under-utilised resource within the NHS, in spite of their skills and experience, and the accessibility of their premises. In recent years, community pharmacists have demonstrated the value of the clinical services they offer, particularly in the prevention of cardiovascular disease (CVD).