Volume 5, Supplement 1, September-October 2008
A round table meeting for practice nurses: 7 July 2008, London
Best Practice Principles for Cholesterol Lowering
Volume 4, Supplement 1, May-June 2007
Omega-3 fatty acids: Optimising their use in cardiovascular disease and diabetes
Volume 7, Supplement 2, Jul-Aug-Sep 2010
Navigating the new NICE guideline on type 2 diabetes: finding the best treatment pathway for each patient
The new NICE guideline enables us to individualise care bearing in mind the needs of the person in front of us. It is concerned with clinical efficacy, and – for once – the cost of care has not noticeably influenced its recommendations. In contrast, QOF does the exact opposite, demanding that we drive our patients’ HbA1c down to low […]
Why doesn’t telling people what to do work?
I hate being told what to do and usually I will do the opposite. So where on earth did I get the belief that I know what is right and that I must make sure I tell everyone what to do to stay healthy?
Living with frailty: A guide for primary care
Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their in-built reserves. This means the person is vulnerable to dramatic, sudden changes in health triggered by seemingly small events such as a minor infection or a change in medication. BJPCN, Volume 12, Special Issue 1, Jan-Feb-Mar […]
A tool kit for the diabetic foot
Diabetes clinics form a major part of the workload for practice nurses, but 95% of routine diabetes care is delivered by patients themselves or by family members and carers. It is imperative that we offer people with diabetes concise, up-to-date education for effective foot care and to prevent complications.
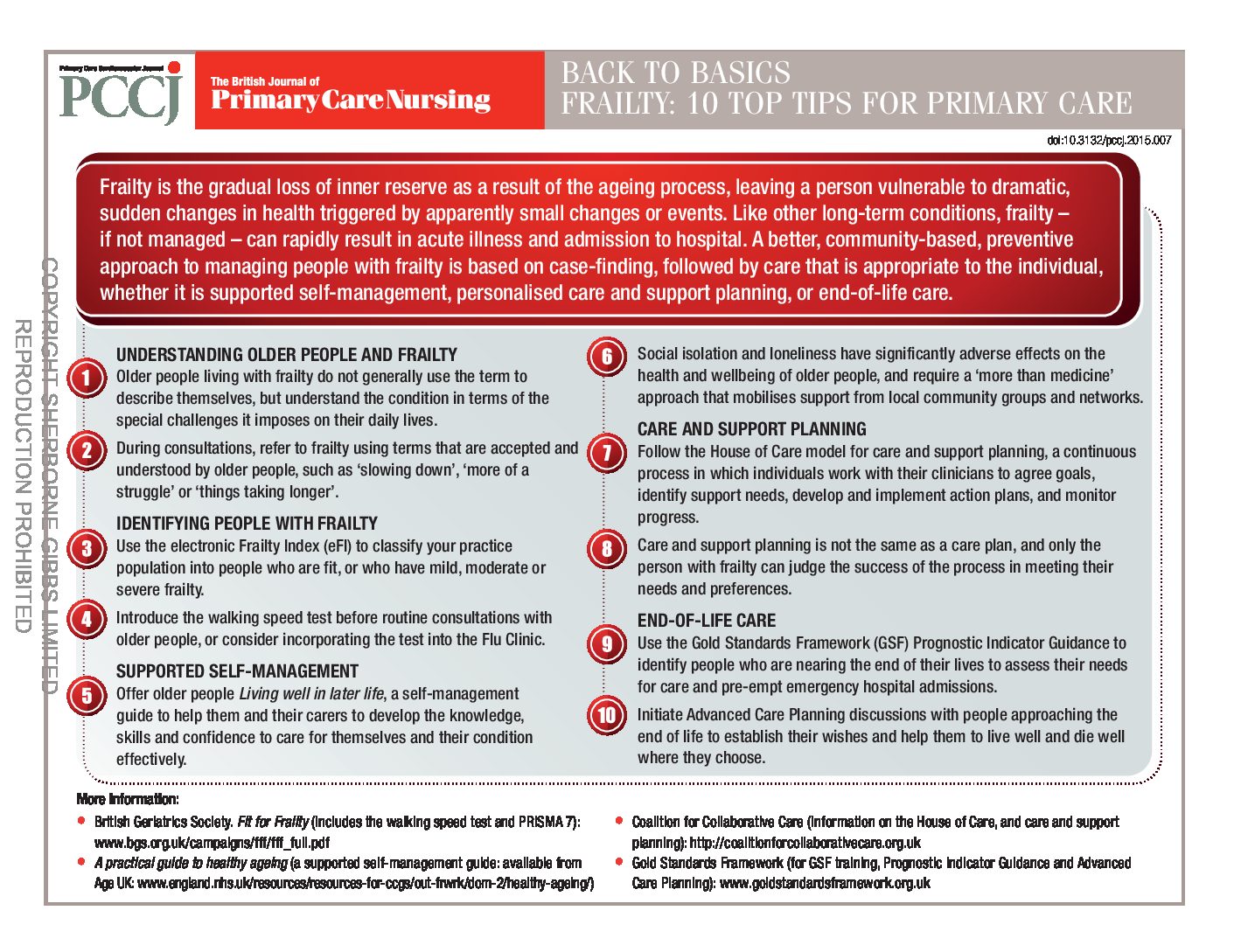
Back to Basics: Frailty – top 10 tips for primary care
Frailty is the gradual loss of inner reserve as a result of the ageing process, leaving a person vulnerable to dramatic, sudden changes in health triggered by apparently small changes or events. Like other long-term conditions, frailty – if not managed – can rapidly result in acute illness and admission to hospital. A better, community-based, preventive approach to managing people with frailty is based on case-finding, followed by care that is appropriate to the individual, whether it is supported self-management, personalised care and support planning, or end-of-life care.
Understanding frailty as a long-term condition
A commonly heard clinical expression is “He/she is very frail”. It provides a summary statement of an older person that implies concerns over vulnerability and prognosis. This is how we have conventionally considered frailty—as a descriptive label: ‘the frail elderly’. In this article, we will re-frame frailty in a potentially more helpful way. We will examine frailty from the perspective of an abnormal health state that behaves just like a long-term condition. This conceptualisation of frailty opens up new approaches to helping people who are frail.
Introduction to frailty
Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their in-built reserves. This means the person is vulnerable to dramatic, sudden changes in health triggered by seemingly small events such as a minor infection or a change in medication.
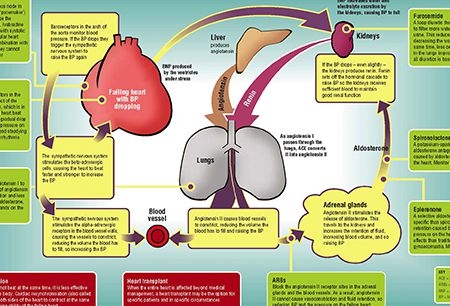
Back to Basics: Treatments for heart failure
A really useful reference for your practice, this handy Back to Basics tells you all you need to know about heart failure treatments.
Heart failure guidelines: Causing confusion in primary care
Chronic heart failure (CHF) continues to be a leading cause of death and readmission to hospital in the UK. Since the availability of specialist CHF services is variable, many patients rely on practice nurses to review their care. The National Institute for Health and Care Excellence (NICE) guidelines have proved very helpful, but are now a cause for confusion as new evidence changes the management of heart failure.