Patients with chronic conditions such as heart disease or diabetes need to plan carefully before travelling long distances and taking holidays. Lifestyle changes can have an important impact on disease control, but a bit of thought and preparation beforehand should ensure that your patients’ holidays are both happy and healthy.
Calculating cardiovascular risk score
Diagnosing diabetes
The number of people with diabetes in the UK is almost 1.8 million and this is continuing to rise, according to recent figures. But only about half of these are currently diagnosed. It is obviously essential to ensure that these people are diagnosed as early as possible and then managed appropriately to ensure they receive the best possible care to minimise long-term complications. In this article, we review how to diagnose diabetes accurately, based on good practice recommended in standard two of the National Service Framework (NSF) for Diabetes. What should we be measuring in people who present with the classic symptoms and in those who do not to ensure an accurate diagnosis of diabetes?
Healthy eating for type 2 diabetes: let’s go shopping
People with diabetes used to be advised to watch their carbohydrate – particularly sugar – intake. But dietary recommendations have developed over the past few years so that they are now similar to the healthy diet that we should all be eating. Are there any remaining differences in what we should be telling patients with diabetes about their diet? Fewer than you might think. In this article we take a ‘supermarket tour’ that explains what patients with diabetes should be putting in their trolleys and what they should be leaving on the shelves.
Changing practice in hypertension: ASCOT win for newer antihypertensives
The British Hypertension Society Guidelines published last year were widely welcomed as a major step forward in the management of patients with high blood pressure. In common with all recent guidelines they were based on a review of all relevant evidence, mainly gained from clinical trials. However, medicine is never static and research is ongoing. A major study – ASCOT – has provided new information about the benefits of newer combinations of antihypertensives compared to older drugs. What did the study show and how should we act on the results to improve outcomes for our patients?
Isolated systolic hypertension
Isolated systolic hypertension (ISH) – an increase in the higher of the two numbers when blood pressure (BP) is measured – is the commonest type of high BP in older people over the age of 60. The systolic pressure used to be dismissed as less important than the lower number – diastolic BP – but studies have shown that it is associated with increased risk of cardiovascular disease. ISH accounts for up to 75% of the overall incidence of uncontrolled hypertension in the elderly and appears to be more common in women than men.
How to score top marks for secondary prevention of coronary heart disease
In this second article in our series on the Quality and Outcome Framework (QOF), we will discuss how to maximise points in the secondary prevention of coronary heart disease (CHD) and heart failure. This will include lipid management and smoking cessation.
One year on: boldly going where no primary care nurse has gone before
Welcome to the first year anniversary issue of the British Journal of Primary Care Nursing (BJPCN). It has been an eventful year for primary care nurses, with new challenges coming from all directions. In each issue of the journal we have tried to provide practical information and tools to help you find your way through the expanding universe of primary care in cardiovascular disease and diabetes – to boldly go where no primary care nurse has gone before!
Chewing the fat
Some fat is essential for maintaining good health, in order to provide essential fatty acids and the fat-soluble vitamins A, D, E and K. Essential fatty acids can only be derived from foods because they cannot be synthesised by the body. However, the hard truth is that essential fatty acids represent only a very small amount of total energy needs and most people still consume too much fat. How much fat should we be eating? What is the difference between different types of fats and what advice should we be giving patients about fats to reduce their risk of cardiovascular disease?
Measuring BP at home
Most people with hypertension are diagnosed and managed on the basis of blood pressure (BP) measurements taken by healthcare professionals in the surgery. Although clinic readings remain the accepted method of measuring and monitoring BP, they are widely acknowledged to be prone to inaccuracies, such as the infamous ‘white coat effect’ that can lead to artificially high readings. In addition, the relatively small number of readings generally taken in the clinic offers only a ‘snapshot’ look at BP levels that may not reflect real values. There is increasing evidence that the use of self BP measurement – with patients monitoring their own BP at home – may provide some advantages over BP measurement in the clinic or surgery. These include potentially more accurate readings and average values that are more reproducible and reliable than traditional clinic measurements. In this article we look at the evidence for the use of home BP monitoring and the accuracy of home monitors.
What to tell your patients about statins
An increasing number of patients are prescribed statins because of the growing evidence that they can dramatically reduce cardiovascular events. However, the withdrawal of one statin – cerivastatin – some time ago may have made some patients concerned about their safety. What should we be telling patients about the benefits of statins, how long they should take them for and whether there are any risks with these widely used agents?
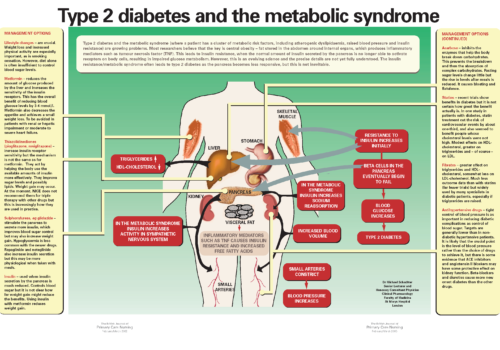
Back to Basics: Type 2 diabetes and the metabolic syndrome
Type 2 diabetes and the metabolic syndrome (where a patient has a cluster of metabolic risk factors, including atherogenic dyslipidaemia, raised blood pressure and insulin resistance) are growing problems. Most researchers believe that the key is central obesity – fat stored in the abdomen around internal organs, which produces inflammatory mediators such as tumour necrosis factor (TNF). This leads to insulin resistance, when the normal amount of insulin secreted by the pancreas is no longer able to activate receptors on body cells, resulting in impaired glucose metabolism. However, this is an evolving science and the precise details are not yet fully understood. The insulin resistance/metabolic syndrome often leads to type 2 diabetes as the pancreas becomes less responsive, but this is not inevitable.