The revised new GMS contract recommends that we screen patients with coronary heart disease (CHD) and diabetes for depression. This is evidence-based, as we know that people with long-term conditions are at high risk of anxiety and depression; but who is going to do it, how is it done and when do we find the time? It would seem obvious to include some sort of screening process in the annual CHD or diabetes review – but is this feasible? In this article we review practical ways of screening for depression in patients with CHD and diabetes.
Screening for Depression in the Cardiovascular Disease Clinic
Functional Foods: More Than Just Good To Eat
There has been a flurry of interest in functional foods over the past few months. Health claims range from lowering cholesterol to improving vitality. Functional foods have been popular in the Far East for many years but only arrived in the UK six years ago. They are now the most rapidly growing sector of the food industry, with estimates suggesting we currently spend around £1 million on them every day. To make informed choices, consumers and health professionals need to know the truth behind the hype. In this article we review the range of functional foods now available, take a look at the evidence for their claims and explore the pros and cons of using them.
Apples and Pears: Targeting Abdominal Obesity
Healthcare professionals spend a great deal of their time screening for, and treating, silent killer diseases such as diabetes, hypertension and hyperlipidaemia but often ignore the primary cause of these conditions, which is often – quite literally – staring them in the face. Obesity can be seen without the need to use any fancy gadgets – we simply need to use our eyes each time we see a patient. There are essentially two main body shapes – apples and pears – each associated with different distributions of body fat. Pearshaped people carry most of their excess fat around the hips, buttocks and thighs. Apples carry most of their excess body fat around the middle; this is known as central obesity and is much riskier for diabetes and cardiovascular disease. In this article we review why central obesity matters, how to measure it and management strategies.
Type 2 diabetes in south Asian communities in the UK
People from ethnic minorities may not get the diabetes care they need because of issues associated with language, literacy and culture, warned a recent Audit Commission report on diabetes – Testing Times. This article explores these issues and gives some insight into the challenges of looking after South Asians – Bangladeshis, Pakistanis, Indians and Sri Lankans – with diabetes, as well as offering some pointers to improve their care and treatment.
Keep taking the tablets: achieving adherence in type 2 diabetes
Most patients with type 2 diabetes require many tablets to control their diabetes and prevent cardiovascular complications. Patients are often prescribed two or three antidiabetic agents, two or three antihypertensives, one or more lipid-lowering tablets and low-dose aspirin. Research has warned that fewer than 50% of patients take their prescribed diabetes medication adequately. The consequence of this poor adherence is increased risk of cardiovascular complications. How do we help patients to take their tablets and so improve their health and long-term outcomes?
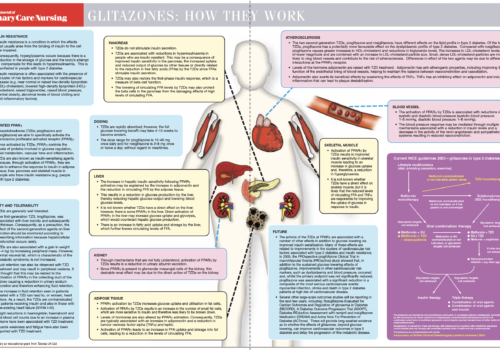
Back to Basics: Glitazones: how they work
Monitoring kidney function in the surgery
The most common cause of chronic kidney failure is diabetes, which accounts for between 30 and 40% of all cases. Chronic kidney disease is a long-term condition usually taking between fifteen and twenty years to reach the final stages. Although 30% of all people with type 2 diabetes will develop some degree of kidney disease, only a minority go on to develop end-stage renal failure. In this article, we look at the benefits of early detection and treatment in slowing the progression of renal impairment.
The role of dietary fibre in optimising health
The gastrointestinal tract plays a vital – and sometimes overlooked – role in maintaining overall health. Dietary fibre, eaten as part of a balanced diet, helps to ensure effective functioning of the intestines and can offer benefit in terms of the prevention and treatment of a number of health problems. As levels of obesity in the population continue to escalate, research has shown that dietary fibre has an important role in satisfying appetite and in weight management, in addition to playing a potential role in controlling insulin levels.
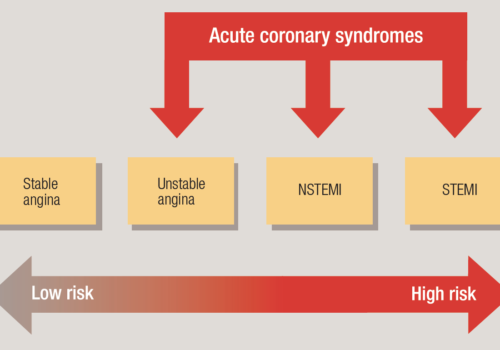
Acute coronary syndromes
Acute coronary syndromes (ACS) include common and high-risk conditions such as unstable angina, which can be difficult to diagnose, particularly in women, the elderly and diabetics. Early identification and appropriate management can significantly reduce the risk of death, morbidity and subsequent hospital admissions. This article aims to clarify what happens in ACS, how they present and how they should be managed.
Editorial
Welcome to the latest issue of the British Journal of Primary Care Nursing (BJPCN). The NHS is currently in meltdown around the ears of primary care teams, with new mergers and reshuffles. There is great uncertainty about who will lead the new PCTs and the structures that will support the delivery of CHD and diabetes care. But, like many of you, I have been around long enough to know that things ‘go in circles’.
Validating and maintaining your CHD register
Disease registers are essential for practices to optimise the diagnosis, management and follow-up of patients with a particular condition, in addition to being an important feature of the Quality and Outcomes Framework. Practices are responsible for demonstrating that they have systems in place to maintain a high-quality register. In this article, we look at a ‘recipe’ for validating a coronary heart disease (CHD) register – but the same method used for validating and maintaining the register can apply to any disease, using appropriate diagnostic and treatment information.