As we reach the end of the year, BJPCN looks back at the challenges that
have been met in the care of patients with respiratory and allergic disease
over the past few years and looks forward to the new situations we will
have to face in the coming year. I have really enjoyed launching this
exciting journal and wish Monica Fletcher, Chief Executive of Education for Health, the very best as she takes on the editor’s role from the next issue.
Symbicort® (budesonide/formoterol) Maintenance and Reliever Therapy – Symbicort SMART® – A new approach to asthma management
Nurses know from first-hand experience that although asthma treatment has come a long way over the past few years, many patients with asthma remain uncontrolled. This results in unscheduled hospital appointments for patients and unnecessary limitations on their lifestyle.
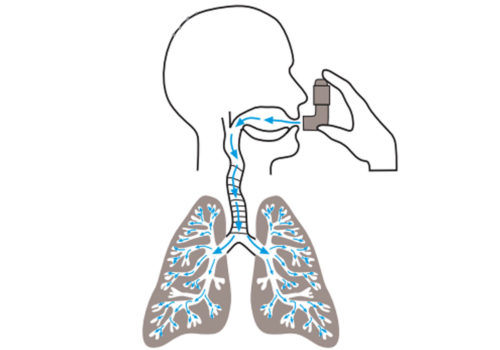
Why Optimise Inhaler Technique in Asthma and COPD?
Asthma UK estimates that 2.1 million patients in the UK are suffering unnecessarily because
they do not use their asthma treatment effectively. This article looks at how inhaled
therapies are deposited in the lungs, and at the basic differences between inhalers – with
a focus on optimising inhaler technique.
The effects of the weather on COPD
Those of us working with patients suffering from COPD know anecdotally that cold
weather directly impacts exacerbation rates and hospital admissions in the same way
as thunderstorms affect those with asthma (see BJPCN Vol 1, Issue 2, March 2007).
This article explores the links between COPD and weather patterns. You may not want
to be thinking about the winter but action now should give time to put preventive systems in
place to help at-risk patients before the cold weather appears again.
Representative sampling – take your pick
How to Treat Winter Coughs and Colds
The number of respiratory consultations in primary care increases in the winter months.
We see more patients with acute exacerbations of their underlying respiratory condition,
such as asthma or chronic obstructive pulmonary disease (COPD) caused by the cold
weather and the increased number of viruses and airborne infections that occur at this
time of year. So what advice should we give to patients with cold and flu-type symptoms during
the winter? And is the approach we take with respiratory patients in any way different from the
approach taken with otherwise healthy individuals?
Editorial Summer
Summer is here and time for a new issue of the BJPCN – packed full of
useful information and news from the respiratory and allergy world.
We cover a lot of different topics in the main articles this month – from
pleural effusions to angioedema, from asbestosis to urticaria. A scan
through the summaries of the latest research in the Evidence in Practice
section will reveal interesting studies with dogs, trees and alcohol! Have
a great read.
Education for Health – Pioneering Primary Care Education 1987-2007
Over the past 20 years, Education for Health and its previous organisation The National Respiratory Training Centre, has provided immensely valuable training support for primary healthcare professionals, particularly in the management of long-term diseases. From small beginnings the organisation has developed into a world leader in nurse training and is actively sharing UK quality and […]
Chronic Kidney Disease – Promoting Self-Management
This article will discuss the evidence for the self-management of long-term conditions, with a focus on chronic kidney disease (CKD). Self-management of CKD can include activities to control and manage blood pressure (BP); changes to diet such as reduced salt intake; smoking cessation; and understanding of the action and side-effects of prescribed medicines.
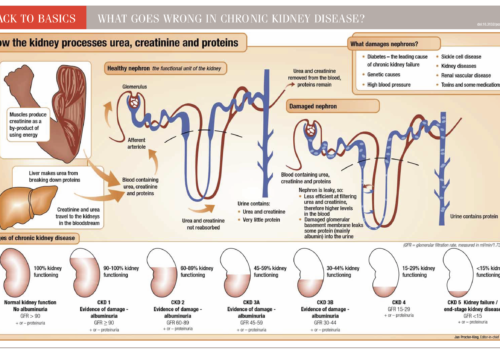
Back to Basics: What goes wrong in chronic kidney disease
Vascular Risk Checks in Patients with Chronic Kidney Disease
Improving Organ Donation Registration in Primary Care
Organ transplants can save or dramatically improve lives, yet figures for 11 February 2009 showed there were 7,903 people in the UK still on waiting lists for transplants, with the majority waiting for a kidney transplant. Last year, more than 400 people died while on the transplant waiting list.