Chronic obstructive pulmonary disease (COPD) is the term used to describe a range of
chronic chest conditions, including chronic bronchitis and emphysema. COPD is
characterised by permanent damage to the lungs and as the condition develops, people
experience increasing breathlessness, to the point where even everyday activities such
as getting dressed or walking up stairs become difficult. This article describes the impact of
COPD, explores the value of exercise in COPD management and discusses possible reasons for its
widespread under-use as effective symptom control.
Bronchodilators in Children with Asthma
Asthma is a common condition in children, with approximately one in eight youngsters in
the UK receiving treatment for asthma at any given time. The British guidelines on the
management of asthma have separate pathways for children of different ages, for those
under 5 and for children aged 5-12 years. In this article, we review some of the
challenges of treating children with asthma, in particular, the best use of bronchodilators.
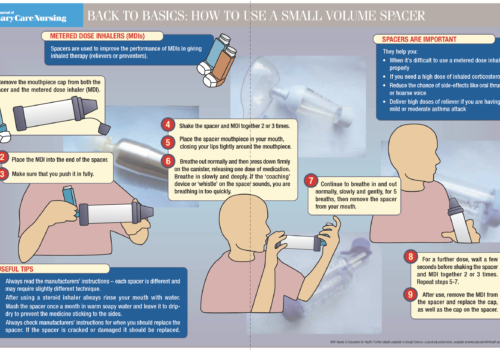
Back to Basics: How to use a small volume spacer
Treatments for Hayfever
Over the next few months practice nurses are likely to see many patients with hayfever
(also known as seasonal allergic rhinoconjunctivitis). Although it may appear to be a
minor complaint, hayfever can result in considerable suffering for the individual, who
may or may not seek professional help and advice. Practice nurses play an important
role in improving the management of this condition. In this article, we describe the impact of
hayfever on patients and provide a comprehensive review of the treatments currently available
for hayfever.
Selecting the correct over-the-counter medicines for hayfever
Hayfever, or seasonal allergic rhinitis, is a condition that patients often present with to their
pharmacist. However, unlike most minor ailments, hayfever is a persistent and recurrent
condition which can have a significant negative impact on quality of life.1 As such, the
correct diagnosis and product selection is essential. The variety of preparations available for the
treatment of hayfever, both over-the-counter (OTC) and on prescription, was discussed in detail in
an earlier edition of BJPCN.2 This article will focus on the options available to community
pharmacists for OTC treatment of hayfever.
Managing pleural effusions in primary care
Patients with recurrent pleural effusions have, to date, mainly been cared for in hospital.
Many have had to undergo repeated hospital admissions, extended hospitalisation,
discomfort and time away from home. This is particularly the case in patients with
recurrent malignant pleural effusion (MPE). However, new technologies mean that these
patients may be managed by close co-operation between primary and secondary care. This
article describes some exciting developments in the management of pleural effusions in a PCT.
Editorial: Winter, respiratory infections and COPD
What a winter we have had! Many children have seen heavy snow fall for the
first time and London was completely immobilised due to the weather. At the
same time our hospitals have been battling to cope with patients suffering with
respiratory infections and exacerbations of their COPD. GP practices have been
stretched to the limit to cope with the additional burden of coughs and colds.
Building capacity is a real problem for everyone working in the health service and
patients’ demands and expectations continue to grow.
Asbestos and the lung
Although the use of asbestos in this country has been tightly controlled for over 30 years
the incidence of asbestos-related lung diseases has increased dramatically over the
last few years. It is expected that this increase will continue during the next decade.
This article describes some of the different lung diseases caused by asbestos and their
management, and provides a useful clinical background to the issues for healthcare workers in
primary care.
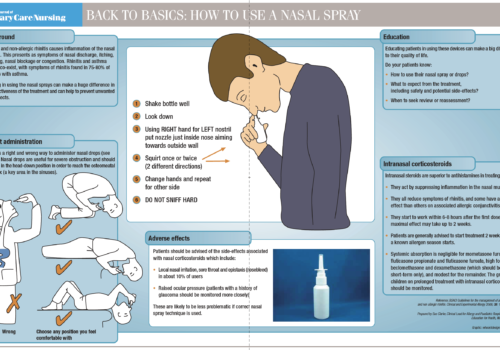
Back to Basics: How to use a nasal spray
Travel tips for patients with respiratory conditions and allergy
Many of your patients will be planning their holidays, but some may be worrying
unnecessarily about their respiratory condition. There are a host of resources and
information available for them, and practice nurses can make sure they provide the
right information about travelling with asthma, COPD or allergies. This article
provides practical tips on how best to advise patients who are thinking of going on holiday.
Scoring Top QOF Points for COPD
Making the most of self-management plans in COPD
The Department of Health’s Expert Patient Programme recognises the role of selfmanagement
in many different disease areas and its report Self Care recommends the
concept of encouraging people with long-term conditions to self-manage where
possible. Diabetes management would never succeed without the active participation of
the person with the condition and asthma management plans have been advocated for some
time for people with asthma. What can self-management plans achieve in chronic obstructive
pulmonary disease (COPD)?