Diabetes affects approximately 3-4% of the British population but is thought to be significantly under-diagnosed. How can we improve the number of patients who are diagnosed early and so improve their risk of long-term complications?
New role for HbA1c in diagnosing diabetes
Glycated haemoglobin – HbA1C, or A1C as it is now being called – should be used to diagnose diabetes, according to a recent recommendation from an international expert committee appointed by the American Diabetes Association, the International Diabetes Federation and the European Association for the Study of Diabetes. We explore the basis for this recommendation, and look at why HbA1C would provide a more accurate measure for diagnosing diabetes than glucose tests and what the change would mean in clinical practice.
Starting on a GLP-1 analogue: Byetta or Victoza
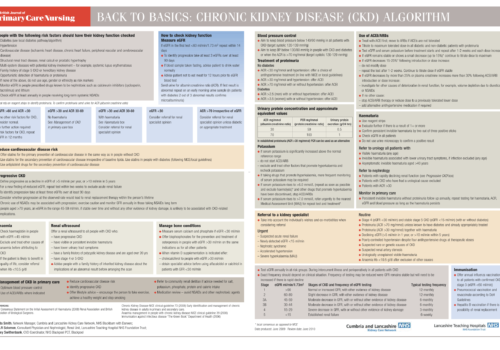
Back to Basics: Chronic kidney disease (CKD) algorithm
Putting the NHS health check programme into action: hearts, brains and kidneys
The prevention of cardiovascular disease (CVD) is being moved up a gear with the ambitious and wide-reaching NHS Health Check programme. The agenda for this programme has been clearly laid out for us in the Putting Prevention First best practice guidance that was published in April 2009. The “Cog Man” on the cover highlights the close links between the heart, brain, kidneys and diabetes, explaining the comprehensive nature of vascular risk assessment, and this image is going to be seen regularly on national leaflets and posters promoting the programme. This article provides a practical guideline for the primary care team on implementing the Health Check programme, setting out who we should be checking, what we should be checking and how we should act on what we find.
Helping your patients to manage their weight: a behavioural approach
The health risks of obesity are only too obvious but, despite this, its prevalence continues to increase. It is a leading cause of both physical and psychological ill health, and is notoriously difficult to treat. For this reason, the National Institute for Health and Clinical Excellence (NICE) emphasises the importance of preventing obesity and has produced guidelines on the most effective approaches. Many health professionals wish to support their patients with weight loss, but research has shown that they do not always feel well equipped to do this. In this article we review the importance of a behavioural approach in managing overweight and obesity and provide practical advice on how to help overweight patients achieve sustainable behavioural change.
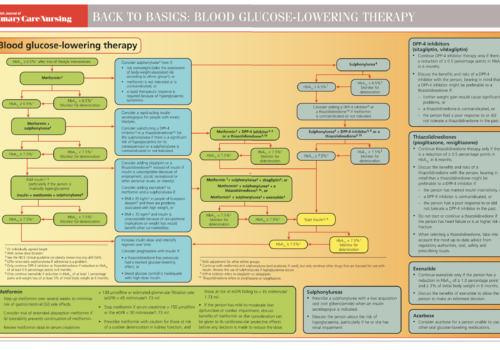
Back to Basics: Blood glucose-lowering therapy
New drugs and where they fit in the treatment algorithm
In May 2009, NICE published recommendations on the use of newer agents for the control of blood glucose in type 2 diabetes. This guideline provides a partial update for NICE Clinical Guideline 66 on the management of type 2 diabetes that was published last year. These newer agents include the dipeptidyl peptidase-4 (DPP-4) inhibitors, thiazolidinediones (TZDs), the glucagon-like peptide-1 (GLP-1) mimetic exenatide and the long-acting insulin analogues (insulin detemir and insulin glargine).
Chronic kidney disease: Helping practices to identify patients at risk and reduce progression
Chronic kidney disease (CKD) has moved rapidly up the healthcare agenda over the last few years. It has shifted from being considered as a rather nebulous condition of interest mainly to nephrologists to the front line of chronic disease detection and prevention in primary care as part of integrated management of vascular risk. In fact, […]
Standing up, sitting or lying down: what do these BP readings mean?
Maintaining a healthy blood pressure (BP) is important in preventing cardiovascular events such as heart attack and stroke, and measuring BP is a key step in cardiovascular risk assessment. However, it is not always measured correctly. Readings should be taken from both arms and the higher reading of the two, if there is a difference, should be used and a record should be kept of the preferred arm for future readings. But what about the patient’s position? Does a lying and standing measurement need to be done in all patients? What is an ‘acceptable’ difference? And does it matter?
Making sense of HDL cholesterol in cardiovascular risk
Lowering LDL cholesterol (LDL-C) with statins for the prevention of cardiovascular disease (CVD) has rightly become a core activity for primary care health professionals. However, despite effective lowering of LDL-C, many patients still suffer cardiovascular events. Experts have called this ‘the residual risk’ and have speculated whether further cardiovascular events can be prevented by attention to other lipoprotein fractions, particularly HDL cholesterol (HDL-C).
Helping patients with diabetes to win the battle to control their weight
Many people with type 2 diabetes are overweight or obese at diagnosis and continue to struggle to control their weight. This article looks at why people with diabetes find weight control more of a challenge than the rest of us and how practice nurses can help patients to remain positive, particularly when starting insulin to optimise blood glucose control.