Supraventricular tachycardia (SVT) often begins in childhood or early adulthood. In this review, a patient describes her experience of coping with episodes of SVT and the experience of undergoing cardiac ablation and subsequently having a pacemaker fitted.
Editorial
Welcome to the latest issue of BJPCN, which we hope you will see as a bunch of spring flowers, offering a bouquet of delights to cheer you on your way to meeting the challenges of providing the best care for patients with cardiovascular disease and diabetes.
Taking the heartache out of angina
Angina is common, particularly among older people. It affects around one in ten women and up to one in five men aged 65 and over. The good news is that the outlook for patients with stable angina is relatively good as long as we help them to take appropriate prevention measures. Unstable angina has a more variable prognosis, but effective prevention can again help to reduce the risk of heart attack. How can we optimise the diagnosis and ongoing care for the many people in our practices with angina?
Palpitations: careful assessment reduces the time to diagnosis
Palpitations are a common presentation in general practice and a frequent reason for cardiology referrals. They generally cause considerable distress and anxiety to the patient and can also evoke feelings of uncertainty in the health professional consulted, but the good news is that palpitations are often benign. The skill lies in identifying patients with a significant heart rhythm abnormality that could be helped by treatment and those at risk of adverse outcome. This can be achieved by taking a careful history and simple investigations.
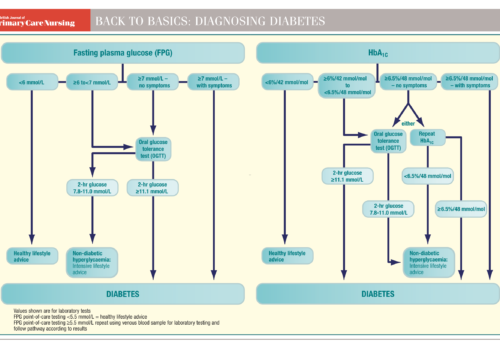
Back to Basics: Diagnosing diabetes
Providing the best care for patients with leg ulcers
Over the years, many of the conversations I have had with patients and nurses have been about leg ulcers. It seems that there is a fear or stigma about leg ulcers, as if labelling a wound on the lower leg an ulcer will somehow make it harder to heal. In a busy practice it may seem pointless to perform a full assessment on a patient presenting with a small traumatic wound on their lower leg. But it is important to acknowledge the risk of progression from a simple wound to chronic leg ulceration and to assess patients fully for any problems that may influence wound healing or may have contributed to the tissue damage.
Avoiding weight gain after stopping smoking
Stopping smoking is associated with considerable health benefits and large numbers of smokers want to quit. However, concern about weight gain is one of the reasons people often give for not being able to quit smoking. It often reinforces the decision to continue smoking, particularly in women and young people who may mistakenly believe that smoking is an effective way to control their weight. Even if an individual successfully quits smoking, weight gain can often be the factor that causes relapse. What can we do to help?
What you need to know about having an oral glucose tolerance test (OGTT)
This leaflet is intended to provide information for people who have been advised to have a glucose tolerance test. It is very important to follow the guidelines given below so that your test is accurate and you don’t need to repeat it.
Editorial
Welcome to the first issue of BJPCN for 2010 – a new year and a new decade! How are you doing on your New Year’s resolutions? I have recently lost quite a bit of weight and feel so much better, both physically and mentally. This has prompted me to reflect on how people decide to change and how they act on that decision, so I would like to share some of my thoughts and the approach I have adopted as a result.
Beta-blockers in heart failure: are we doing the best we can for our patients?
Since the first description of a beta-blocking agent in 1962, this class of drug has become among the most widely used in the management of cardiovascular disease (CVD). Betablockers are now used routinely after a myocardial infarction, in patients with angina pectoris and as an additional therapy in the management of high blood pressure. However, they have traditionally been avoided in heart failure because it was thought that they were potentially harmful. But some large, well-designed randomised controlled trials have provided an overwhelming body of evidence to dispel this myth once and for all.
Selecting targets in cardiovascular risk reduction: guidelines or indicators?
There is a profusion of guidelines and recommendations setting out targets for managing the risk factors associated with cardiovascular disease to help us manage our patients. But which ones should we follow? In this article, we compare the treatment thresholds and targets in these different recommendations, consider the reasons for the variety of targets and look at how to rationalise the selection of the targets for an individual patient.