What are the practicalities of supporting people with diabetes who fast during Ramadan? Practice nurses can make a real difference by educating patients before Ramadan starts and advising them on what they need to consider before starting their fast. Patients need to be involved in the whole process so that they are well aware of the importance of managing their diabetes to ensure good control of their glucose levels throughout Ramadan. We review how to assess patients before Ramadan, what adjustments to make to medication and how to follow up.
Caring for your diabetes during Ramadan
Fasting during Ramadan means that you have longer gaps between meals than usual. Many people also eat more food in one meal – in particular, more carbohydrate-rich and fatty foods – during this time. If you have diabetes, this may mean that you have large swings in your blood sugar levels during Ramadan. During the day – when you are fasting – your blood sugar is likely to drop. This may make you feel weak, tired and dizzy. This is called hypoglycaemia (which means low sugar) – a period of hypoglycaemia is sometimes called a ‘hypo.’ People who are sick or whose health may be adversely affected by fasting – such as those with diabetes – do not have to fast during Ramadan. However, some people do decide to observe the fast. This leaflet gives you some tips on how to keep well.
American College of Cardiology Annual Scientific Sessions
Preventing and treating bone disorders in chronic kidney disease
Chronic kidney disease mineral and bone disorders (CKD-MBD) is a slowly progressive complication of CKD occurring over many years. The kidneys are unable to maintain normal levels of calcium and phosphate and respond to the hormones needed to maintain healthy bones. CKD–MBD is a common problem in people with stage 3 CKD onwards and affects almost all patients receiving dialysis. This article explains why renal bone disease occurs, the problems it can cause for patients affected and provides practical tips on how to identify people at risk and management options.
Moving stroke prevention up the healthcare agenda
“There are lots of really powerful examples around o f things we can do to improve quality while improving productivity”
This statement from Sir David Nicholson, the NHS Chief Executive, appears on the NHS Evidence website, where the recognition and optimal treatment of atrial fibrillation (AF) is given as one of the top six Quality, Innovation, Productivity and Prevention (QIPP) examples from across the entire NHS.
Feeling the pinch: the impact of weight loss surgery on cardiovascular risk
Weight loss (bariatric) surgery is becoming increasingly common as the obesity epidemic continues to flourish, and recent NICE guidelines have supported this approach. In this article, we review the procedures used in bariatric surgery, the impact on patients’ cardiovascular risk and type 2 diabetes, what the guidelines recommend and the long-term care of patients who have undergone this type of surgery.
Transient ischaemic attack: act fast to reduce the risk of stroke
The White Paper, Saving lives: our healthier nation (1999), set out a target to reduce the death rate from coronary heart disease and related illnesses such as stroke by 40% in the under-75s by 2010; recent trends indicate that this target will be met. Although the past forty years have seen a significant reduction in age-standardised stroke mortality rates, stroke still accounts for around 53,000 deaths each year in the UK, with more than 9,500 of these occurring in the under-75s. This article reviews how we might reduce the huge burden of stroke by improving the management of transient ischaemic attack (TIA).
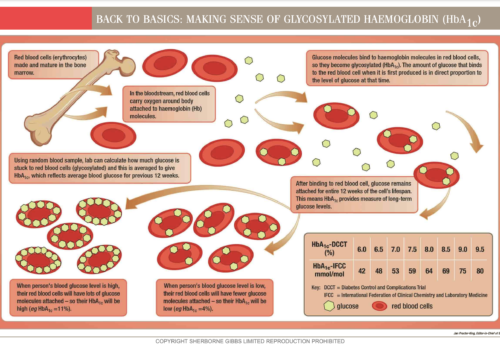
Back to Basics: Making sense of glycosylated haemoglobin (HbA1c)?
Stratifying stroke risk to guide treatment in patients with non-valvular atrial fibrillation
Antiplatelet (usually aspirin) and anticoagulant (usually warfarin) treatments are available to reduce the risk of stroke in patients with atrial fibrillation (AF) but both have potentially harmful adverse effects and warfarin can be time-consuming and expensive to monitor. Guidance exists for choosing between treatments but is often insufficiently detailed to support an informed choice about the risk and benefits. Prescribers and patients are often left with a choice between aspirin or warfarin, and aspirin – which is perceived to be safer and easy to use – is often chosen. This article explores the evidence for aspirin and warfarin in preventing stroke in patients with AF, and describes how we should change the way that decisions about treatment are made.
Thinking yourself free: understanding the principles of cognitive behavioural therapy
How are you feeling? If you had to measure how you feel on a scale from ‘grotty’ through ‘good’ to ‘great’, how would you rate yourself? More importantly, what do you think it was that decided how you feel today?
Drug treatment for atrial fibrillation
Irrespective of whether the atrial fibrillation is constant or occurs in paroxysms, that is, it is intermittent, the decision to administer antiplatelet drugs or anticoagulants should depend on the patient’s cumulative risk factors. These risk factors include age and previous medical history.
Looking to the future for the management of AF and prevention of stroke
Atrial fibrillation (AF) is becoming an epidemic, affecting 1% to 2% of the population in the developed world. Looking to the future, the prevalence of AF will grow dramatically in the coming decades as the elderly population increases. The growing numbers underline the need to improve the detection of patients with AF and measures for reducing their risk of stroke.