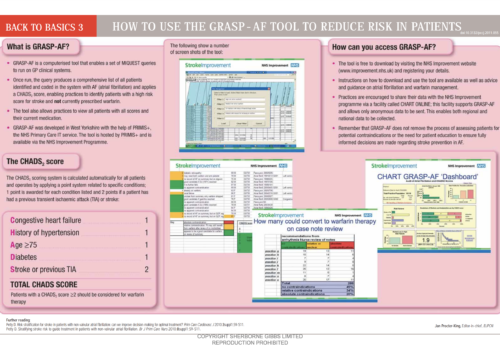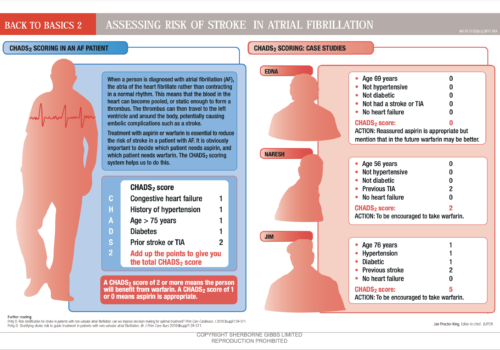
Back to Basics: How to use the GRASP – AF tool to reduce risk in patients
Proteinuria: should it replace cholesterol as a marker for people at high risk of CVD?
We have all seen paintings of early physicians looking at flasks of urine to give an indication of a person’s health. And most of us can remember days of rows of urine pots lined up to test for new patients in primary care and in hospital outpatient clinics. We may assume that those days have gone in the era of blood testing and CT scans. So why are we suggesting that urine testing has a central role in finding patients with previously undiagnosed cardiovascular disease?
Editorial – Going back to basics in cardiovascular disease
There are 28 cardiac and stroke networks in the country. They play an important part in implementation of national strategies, enabling high-quality services to be planned and delivered to patients within the framework of primary and community care. One of the most useful contributions of the networks is provision of education and training for primary care staff. The “Back to Basics” material in this supplement forms the backbone of what is presented at study days. The articles cover some of the most common cardiovascular conditions that are seen in primary care, showing clearly what causes the symptoms, how best to assess and manage patients, and how the treatments actually work. They help healthcare workers both to understand these conditions and to explain them to patients, and therefore really improve patient care.
Editorial
This educational supplement is brought to you by the Cardiac and Stroke Network. What is this Network, and how can it further support your education and development?
Editorial
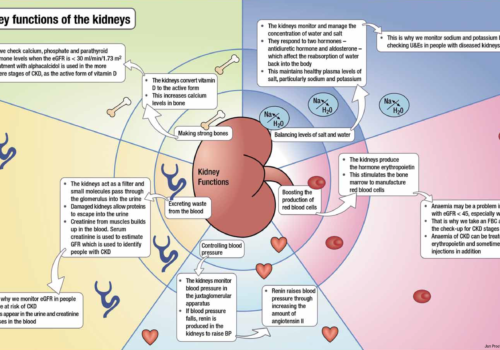
Chronic kidney disease (CKD) has shot up the primary care agenda over the last few years, and is now well recognised as an independent risk factor for cardiovascular disease (CVD). At the same time, CVD is a risk factor for progression of CKD. The close links between CKD and CVD mean we have to get to grips with assessing patients’ kidney function and ensuring those with CKD receive the treatment needed to prevent progression. This special issue devoted to CKD is full of step-by-step guides and illustrated articles to help you get to grips with this important condition.
Editorial
The effective management of long-term conditions such as chronic kidney disease (CKD) is probably the single greatest challenge faced by the NHS. The population is growing and people are living longer. Every week, the life expectancy for a newborn baby in the UK increases by more than 24 hours. While this is, in part, testament to the success of our health services, it also places steadily increasing demands upon them. As the population ages, the number of people living with long-term conditions is predicted to triple by 2050.
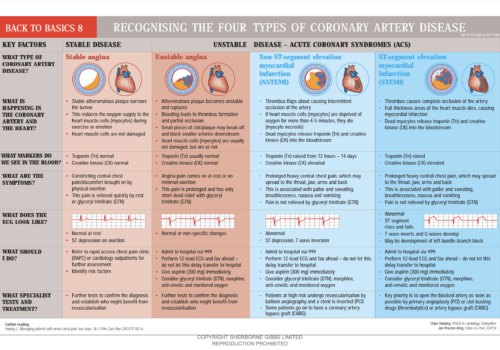
Back to Basics: Recognising the four types of coronary artery disease
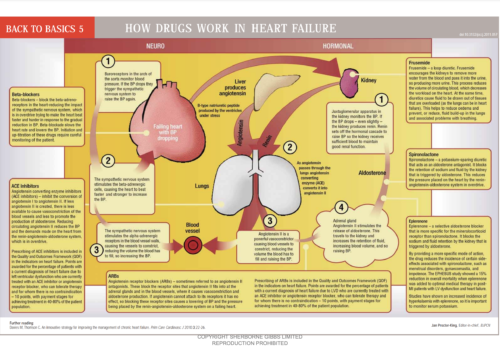
Back to Basics: How drugs work in heart failure
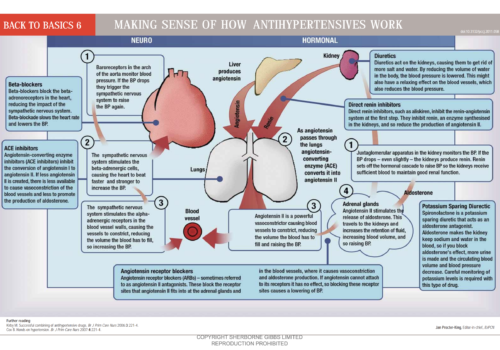
Back to Basics: Making sense of how antihypertensives work
A primary care guide to chronic kidney disease
Chronic kidney disease (CKD) has shot up the primary care agenda over the last few years, and is now well recognised as an independent risk factor for cardiovascular disease (CVD). At the same time, CVD is a risk factor for progression of CKD. The close links between CKD and CVD mean we have to get […]