Ten per cent of the annual NHS budget is spent on medication, with about 75% of this is prescribed in primary care. Ensuring that this money really improves patients’ health is vitally important. As the population ages, more people require increasing numbers of medications for chronic conditions and a third of elderly patients are taking four drugs or more for a spectrum of conditions. But this creates a major challenge – as research reveals that fewer than half of these patients take their medicines as prescribed. How can this challenge be addressed? This new series will provide simple practical guidance on how to conduct an effective medication review for a spectrum of long-term cardiovascular conditions.
It’s as easy as ACD: optimising hypertension treatment
The recent guideline from the National Institute for Health and Clinical Excellence (NICE) on the clinical management of primary hypertension enables us to provide evidence-based care to patients with high blood pressure (BP). The guideline provides a clear treatment algorithm, starting with A (an ACE inhibitor or angiotensin 2 receptor blocker) or C (a calcium channel blocker), depending on the age of the patient, then combining them if target BP is not reached and then adding in D (a diuretic) if required. This article uses a series of case studies to illustrate diagnosis and treatment based on the new guidelines.
Making sense of salt and cardiovascular risk
While salt is an essential part of a healthy diet excessive salt intake is now an important focus for reducing the risk of cardiovascular disease in the UK. It is estimated that reducing everyone’s salt intake to the equivalent of one teaspoon per day would prevent 23,000 deaths from stroke and heart attack each year. Here are practical ideas for helping to achive this goal.
Taking the weight: a primary care team approach to obesity management
Most of the UK population – including the patients we see every day – are now more likely to have a weight problem than be of a healthy weight. Instead of focusing our efforts, and valuable resources, on managing the consequences of obesity, we should tackle its causes and appropriately manage patients motivated to address their unhealthy weight.
In focus: Sight problems after a stroke
Following a stroke up to 60% of people have sight problems, including loss of visual field and trouble with visual processing when the brain no longer makes sense of what the eye sees. Changes to vision can also be a sign of stroke or transient ischaemic attack (TIA). The awareness of visual problems in stroke patients is highlighted in this article which explains the different sight problems and outlines steps which can be taken to help.
PCOS or overweight? Solving the diagnostic dilemma
Polycystic ovary syndrome (PCOS) is the commonest endocrinopathy, affecting 5-12% of women. Every aspect has been controversial from its nomenclature to its management. But accurate diagnosis based on consensus guidelines ensures that treatment can be tailored effectively to each woman’s symptoms and needs.
Editorial
It’s good to talk. Communicating effectively with our patients and their families is a key part of our jobs as primary care nurses and we have a major new communication job on our hands over the next few months. The new guideline from the National Institute for Health and Clinical Excellence makes ambulatory monitoring part of routine practice for diagnosing high blood pressure (BP), so we are going to need to explain to patients why we are sending them home with monitors rather than just taking BP readings in the practice.
Nine processes of care for diabetes
The National Institute for Health and Clinical Excellence (NICE) recommends that all people with diabetes should receive nine key tests at their annual diabetes review. These important markers ensure diabetes is well controlled and are designed to prevent longterm complications. The nine key tests are: weight, blood pressure, smoking status, HbA1c, urinary albumin, serum creatinine, cholesterol, eye examinations and foot examinations. This review discusses the importance of each marker of improved long-term care of patients.
Putting the NICE guideline on ambulatory blood pressure monitoring into practice
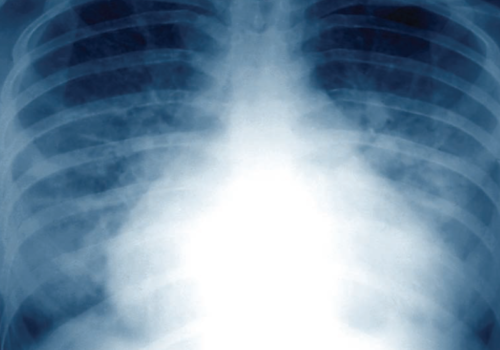
Heart failure: managing breathlessness and oedema
Heart failure is characterised by fatigue, breathlessness and retention of fluid. The update of the National Institute for Health and Clinical Excellence chronic heart failure guidelines has simplified its management by using a stepped approach to investigation and treatment. In this article, we focus on the practical aspects of managing the two main symptoms associated with heart failure – oedema and breathlessness.
One in five strokes warn you they are coming: treat transient ischaemic attacks as emergencies
Transient ischaemic attack (TIA) is a powerful warning sign of an impending, and potentially disabling, stroke. It is important to understand differences between stroke and TIA, how the FAST test can help you recognise the signs, and the use of the ABCD2 score to assess the level of stroke risk. Treating TIAs as emergencies is critically important in preventing a full stroke so urgent referral to your local TIA service is best practice.
Supporting people with communication problems after stroke
Communication problems are one of the most common after-effects of stroke, affecting about one in three people. Losing the ability to speak or understand language – aphasia – is frightening and frustrating. This article offers insights and practical tips to aid communication.