Premenstrual disorders (PMD) are common and have a major impact on the lives of women. Until recently there has been confusion around definitions, leading to difficulties in diagnosis and management. This article describes a new consensus definition and diagnostic criteria for PMD, and advises on the choice of evidence-based treatment.
Made to measure: Tailoring oral contraception to each woman
Individualising choice of oral contraception to each woman is important to ensure safety, and enhance patient acceptability and adherence. However, tailoring should extend beyond simply deciding whether to use a combined or progestogen-only pill. Prescribers should also bear in mind the non-contraceptive benefits of each product, and consider alternative regimens for women with hormone-related medical conditions or those who wish to avoid menstrual bleeds.
Fertility problems
If you have fertility problems, it means you have difficulty in conceiving (becoming pregnant) despite having regular sex without using contraception. Before you begin to worry, remember that many couples take several months to conceive. Over eight in 10 couples conceive within a year of trying, while about nine in 10 conceive within two years.
Practical prescribing to promote urinary continence
Urinary incontinence and related conditions have a high prevalence and a major impact on a patient’s quality of life. Drug therapy can be very effective and forms an important part of the treatment armoury when managing women with incontinence. Unfortunately, medication can be associated with adverse effects, but there are approaches that can be used to maximise a drug’s effectiveness and limit problems that reduce adherence to treatment.
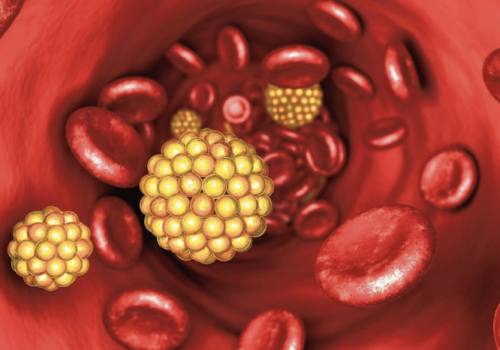
The practical management of patients with dyslipidaemia
The number of deaths each year from cardiovascular disease (CVD) has nearly halved in the UK since the early 1980s. There are many reasons for this success, but 25%-50% of the decline in deaths from coronary heart disease (CHD) can be attributed to secondary prevention in high-risk patients. However, despite the hard work of GPs […]
Healing the sick, advancing the science
“There are two objects of medical education: to heal the sick and to advance the science.”
An update on GRASP-AF
Through the support of NHS Improvement, Guidance on Risk Assessment for Stroke Prevention in Atrial Fibrillation (GRASP-AF) has been rolled out nationally. Nearly 2,000 practices have adopted the GRASP concept, representing an overall population of 13 million.
Suspected VTE and referral outcomes: results of a general practice audit
In-house D-dimer testing and the Wells Score combined meant that cases were referred to secondary care only when patients were strongly suspected to have VTE or pulmonary embolism. Some 86% of VTE cases had properly documented risk assessment.
Time to GRASP heart failure in primary care
Since the introduction of the Quality and Outcomes Framework (QOF), GPs have been incentivised to keep a register of patients diagnosed with heart failure (HF). Such registers are only effective if they are audited regularly, since they are likely to contain errors and omissions. GRASP-HF is a new tool designed to help busy practices achieve a systematic approach to the identification, diagnosis and management of patients with HF.
Nothing stays the same in medicine – or the QOF
“The hardest conviction to get into the mind of a beginner is that the education upon which he is engaged is not a medical course but a life course, for which the work of a few years under teachers is but a preparation.”Sir William Osler (1849-1919), from The Student of Medicine.
12 minutes and the simple seven
Exercise is a preventive tool in combating cardiovascular disease, type 2 diabetes and obesity: an extra 12 minutes a day could make a big difference.
Cardiovascular morbidity and mortality in schizophrenia: implications for primary care
People with schizophrenia have substantial premature mortality compared to individuals without schizophrenia. They also have a wide range of co-morbidities and multiple physical health conditions but are less likely than people without schizophrenia to have a primary care record of cardiovascular disease. This suggests a systematic underrecognition and under-treatment of cardiovascular disease, which may contribute to the increased mortality seen in this vulnerable patient group.