The first section of this supplement made the case to consider frailty from the perspective of a long-term condition. This and the next section explore what this means in terms of applying some of the well-developed models for the care of longterm conditions to people who are living with frailty. First, we examine how the highly evidence-based model of supported self-management might be applied to frailty.
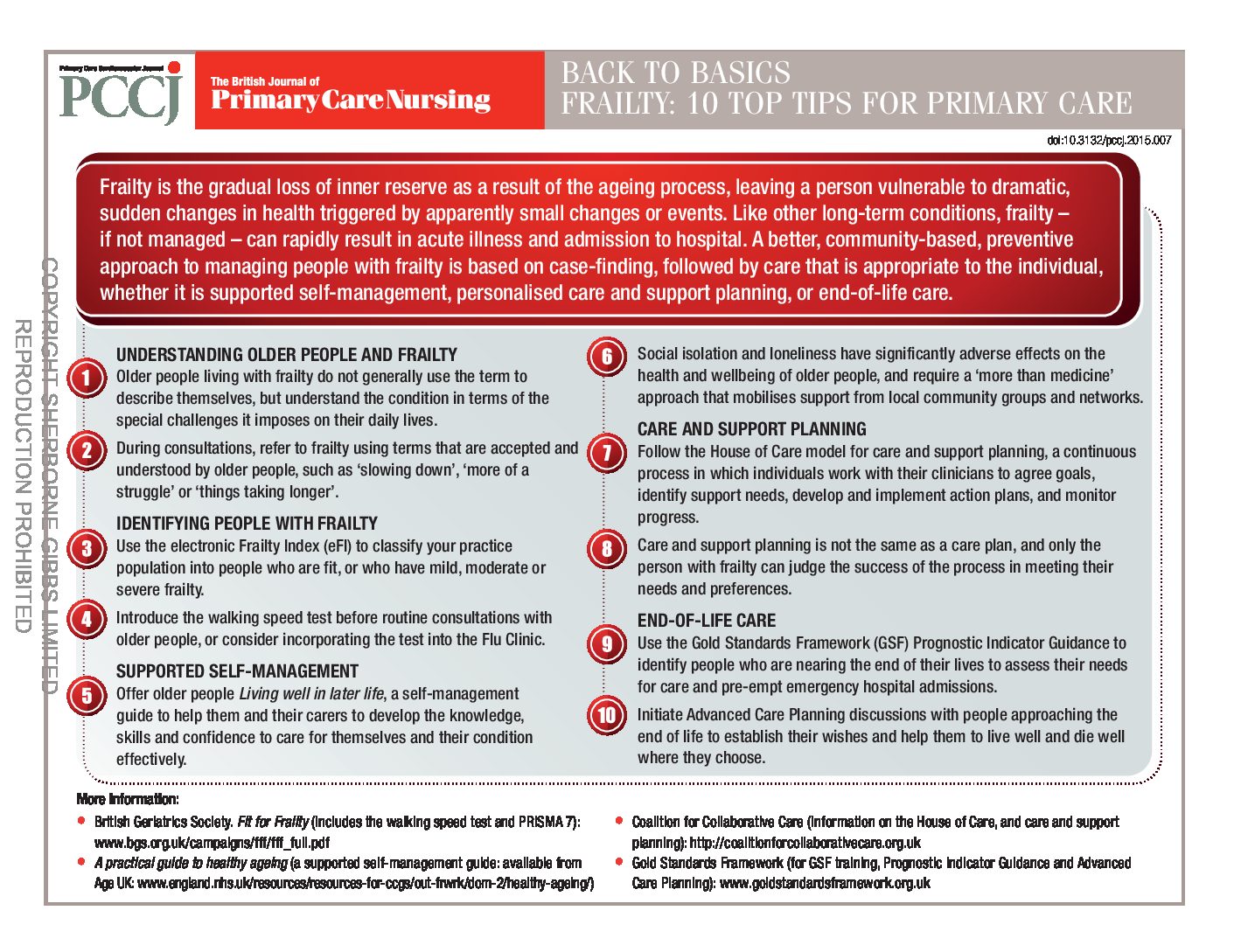
Back to Basics: Frailty – top 10 tips for primary care
Frailty is the gradual loss of inner reserve as a result of the ageing process, leaving a person vulnerable to dramatic, sudden changes in health triggered by apparently small changes or events. Like other long-term conditions, frailty – if not managed – can rapidly result in acute illness and admission to hospital. A better, community-based, preventive approach to managing people with frailty is based on case-finding, followed by care that is appropriate to the individual, whether it is supported self-management, personalised care and support planning, or end-of-life care.
Introduction to frailty
Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their in-built reserves. This means the person is vulnerable to dramatic, sudden changes in health triggered by seemingly small events such as a minor infection or a change in medication.
Understanding frailty as a long-term condition
A commonly heard clinical expression is “He/she is very frail”. It provides a summary statement of an older person that implies concerns over vulnerability and prognosis. This is how we have conventionally considered frailty—as a descriptive label: ‘the frail elderly’. In this article, we will re-frame frailty in a potentially more helpful way. We will examine frailty from the perspective of an abnormal health state that behaves just like a long-term condition. This conceptualisation of frailty opens up new approaches to helping people who are frail.
Blood pressure: A call to action for primary care
Over the next 10 years, an estimated 45,000 quality-adjusted life-years and £850m health and social care costs could be saved, if England saw a 5 mmHg reduction in the average population systolic blood pressure. In addition, substantial reductions in death and disability could be achieved if there was a step change in our approach to detection and treatment of hypertension. This is the rationale behind the Blood Pressure Action Plan that was published recently.
Injection technique: Passing on best practice to patients
In the UK, an estimated 1 million people with diabetes use injectable therapies, and these patients are increasingly being managed in primary care. As a result, more primary care nurses are taking responsibility for the initiation and continuing management of injectable therapies, including advising on and reviewing an individual patient’s injection technique.
Back to Basics: Treatments for heart failure
A really useful reference for your practice, this handy Back to Basics tells you all you need to know about heart failure treatments.
Travel advice for people with heart disease
More people than ever are making trips overseas. Many of us have long-term conditions that we manage with lifestyle choices and medication or medical devices. You may have high blood pressure, angina, a previous heart attack, heart failure or another heart condition. This leaflet will help remind you of some of the advice given to you in a pre-travel consultation with your practice nurse or travel nurse.
Is sugar the new villain? Putting the evidence on trial
For years dieters have been trying to avoid fat, and low-fat products have been promoted as the healthier option. But there is now a great deal of publicity around sugar and its toxic effects on our health, including claims that it is the ‘new tobacco’. The sweet white stuff is being blamed for the obesity epidemic and with it diseases such as diabetes and heart disease. So what is the evidence behind the hype, and what should we as health professionals be advising patients?
Why and when to test for potassium
The World Health Organization has recommended that everyone should be eating more foods that contain potassium, and we routinely measure this electrolyte as part of the standard U&Es blood test. But why is potassium important for our health, and why do we need to worry if a patient’s levels are too high or too low?
Non-alcoholic fatty liver disease under the microscope
Non-alcoholic fatty liver disease (NAFLD) is currently the most common cause of abnormal liver function tests. Current advice is simply to monitor patients’ liver function, but is this really correct? And how do we identify and manage people at risk of developing NAFLD?
Obesity: The harsh reality and new solutions
Practice nurses are in the frontline of the fight against obesity, yet they face a moving target. Around 10 years ago, the ‘centre ground’ of the battle comprised patients with around 10 kg to lose; today, it is 20 kg. This has profound implications for weight management and a range of related conditions, but recent research is highlighting new solutions for this group of patients.