It’s something that we do so often, but are we always doing it the best way? Check out how to measure blood pressure (BP) correctly, with latest advice from the National Institute for Clinical Excellence and the British Hypertension Society.
Making sense of heart failure and its treatment
Heart failure is a high priority in primary care, with the National Service Framework for Coronary Heart Disease, the NICE Heart Failure Guidance, and the new General Medical Services contract quality indicators all setting clear standards for improving the management of patients with this increasingly common condition. This four-page pull-out supplement provides you with a need-to-know, need-to-keep guide.
Disease Focus on… Sleep Apnoea
Sleep apnoea is far more than just snoring associated with brief periods of suspended breathing while asleep. It is an important risk factor for cardiovascular disease and diabetes, so it is well worth asking patients whether they suffer breathing problems during the night and then following up those who do. More than one-third of people with sleep apnoea have hypertension, so measuring blood pressure is important in assessing risk factors and then establishing appropriate preventive treatment.
New British Hypertension Society guidelines tighten cardiovascular risk management
New British Hypertension Society (BHS) guidelines on hypertension focus on cardiovascular risk rather than risk of coronary heart disease, in order to improve the prevention of stroke as well as heart disease.
Maintaining motivation: the long haul of weight loss
There is no doubt about it, achieving and maintaining weight loss long term is a great challenge. Primary care nurses have a significant role in motivating patients to adopt a healthy lifestyle and to persevere with weight management programmes. In the last issue of BJPCN we looked at how to raise the tricky subject of obesity with patients. This time, we continue the issue by exploring how practice nurses ensure a positive working relationship with their patients with weight problems and encourage them as they tackle the long-term issue of obesity.
Improving the primary care management of obesity
Over half of all adults in the UK are overweight, according to latest figures. The number of people who are obese has tripled over the last 20 years, and is still rising. But is weight management an issue for primary healthcare teams? There is clear evidence that it is – with obesity being directly related to increased risk of death and a range of chronic diseases. Obesity reduces life expectancy, on average, by nine years. At long last there is some encouragement for general practices to optimise detection and management of obesity. The new General Medical Services (GMS) contract includes 208 from a total of 1050 points available in the Quality and Outcomes Framework that are affected by weight loss, offering a major financial incentive to general practices to encourage patients to lose weight.
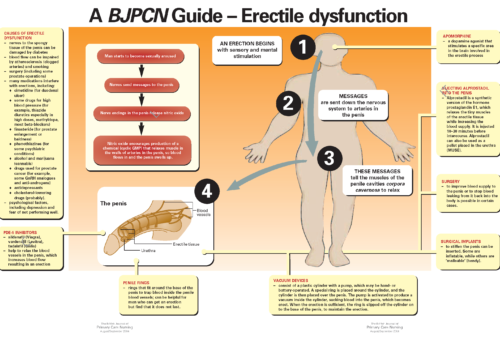
Erectile dysfunction (ED) is a common condition that not only causes distress to a couple, but also indicates the likely presence in the man of cardiovascular and other diseases. By diagnosing and treating ED, nurses can therefore help to restore the coup
Improving the management of diabetic foot conditions
Foot complications are very common in patients with diabetes. At least one in six diabetics develop foot ulcers at some point in their lives. This article reviews why foot complications occur in diabetes, how you can detect foot problems early, and treatment and prevention strategies. The National Service Framework for Diabetes suggests that targeted foot care for people at high risk could save hundreds of amputations a year. By detecting complications earlier, we can make a real difference to patients’ lives, reducing morbidity, improving quality of life and even saving limbs.
Back to Basics: A BJPCN Guide – Erectile dysfunction
New year’s resolutions: take one small step at a time
It’s that time of year again. New Year – time for resolutions, many of which are associated with health. Personal New Year’s resolutions are often about losing weight, getting fit or eating more healthily. All good news for cardiovascular health, the focus of BJPCN. But, as primary care nurses, we could have broader new year’s resolutions, affecting our clinical practice and efforts to improve the health of our patients. Persuading anyone – including ourselves – to change behaviour in an effort to improve health can be challenging at the best of times. The answer seems to be to just take one small step at a time – one that you know you can repeat with ease. Don’t attempt a revolution. In this issue, we offer a range of ideas that you could adopt as ‘new year resolutions’ for your practice – or even yourself!
Raising the issue of obesity with patients who need to lose weight
You know the scenario only too well. Your patient is sat in front of you, taking up more space than he or she used to, and you are discussing the increase in their blood glucose levels. How do you raise the issue of their weight, without offending them or making what seems to them a personal comment?
Tackling the burning issue of smoking cessation
The number of people who smoke has fallen over the past 30 years under a barrage of tobacco control measures, including increasing the price of cigarettes, advertising bans, and health education campaigns. But, one in four premature deaths in the UK (adults aged 35–65 years) are still caused by smoking, and a study published recently warned that today’s smokers puff their way through more cigarettes and start at an earlier age than smokers of fifty years ago. This means that, on average, men who smoke now die ten years earlier than men who don’t smoke. Can primary care make an impact on this ongoing problem? The good news is yes – and the new GMS contract is finally offering us incentives to include smoking in our health promotion activities. In this article, we give you the ammunition to put smoking cessation on your agenda – with the health and economic reasons why it makes sense to help patients quit. Practice nurse Rosemary Evans then explains how she does it in her Docklands practice.