For people with long-term conditions, self-care can have as much, if not more, influence on their health than prescribed medication and treatment. Yet, in many cases, healthcare professionals become frustrated when attempts to improve peoples’ self-care behaviours prove unsuccessful. This article looks at some of the reasons why it can be difficult to encourage people with diabetes or cardiovascular disease to look after themselves effectively; what types of practice can help us to increase people’s success in managing long-term conditions; and how we can incorporate empowering techniques in our day-to-day consultations.
Sex after an MI
Rehabilitation after a myocardial infarction (MI) includes all aspects of a patient’s life – medical, physical and social. Sexual functioning is an important part of most people’s lives. Fears about whether having sexual intercourse could trigger another heart attack is the question many post-MI patients want to ask but embarrassment may stop them. Giving accurate information about sex after an MI is just as much a part of patient education as telling them about cholesterol and blood pressure and can go a long way to helping recovery and preventing further problems such as sexual dysfunction.
Stroke and TIA
Stroke is common, affecting around one in four people over the age of 45 at some time in their lives. Increasing age is a major risk factor for stroke, so the numbers of people suffering a stroke will increase with the ageing population. Primary care teams have a central role in providing effective secondary prevention, but because patients often fall between primary and secondary care, things may be missed. Taking a systematic approach to assessing risk factors, such as blood pressure, and treating them effectively can significantly reduce further stroke risk.
Quality … and beyond
Quality is the latest buzzword in healthcare. The latest GMS contract emphasises this in the Quality and Outcomes Framework (QOF) designed to measure and reward key elements of primary care chronic disease management. In this issue of BJPCN we start a new series – Points mean Prizes – on how to make sure you get all the ticks in the boxes for the data you need to collect to get maximum QOF points. The series will provide a step-to-step guide on how to score on the 76 quality indicators in the 10 clinical domains of care.
Bringing CHD management back to primary care
Managing heart failure effectively in the community Community-based nurses are at the forefront of vigorous efforts to improve the management of coronary heart disease. The Coronary Heart Disease Collaborative is spearheading 30 projects around the country to find practical ways forward. This issue reviews how Durham Dales PCT has brought the management of heart failure firmly back into primary care, with up-to-date registers of heart failure patients and regular clinics in the community.
Chest pain in Primary Care – would you and your team know what to do?
This article considers a possible scenario in primary care in which a patient presents with chest pain. Test yourself to see what you would do. Then check this against our recommendations, reflecting on your current procedures and policies within your practice.
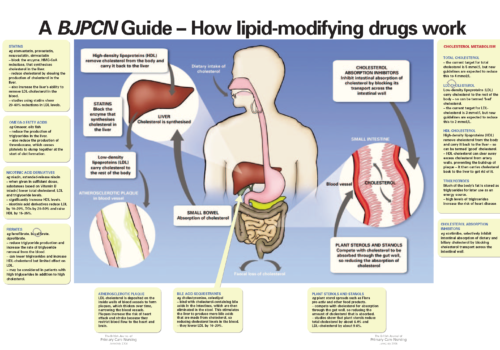
Back to Basics: A BJPCN Guide – How lipid-modifying drugs work
Optimising lipid levels: looking beyond LDL-cholesterol
Treatment with statins is undoubtedly making a major contribution to reducing high-risk patients’ chance of a heart attack or another coronary event. However, their risk remains high, since over half of patients included in statin clinical trials suffered a further coronary event within five years. There is growing evidence that we need to move beyond simply lowering low-density lipoprotein cholesterol (LDL-C) and optimise the whole lipid profile.
Disease Focus on… Sleep Apnoea
Sleep apnoea is far more than just snoring associated with brief periods of suspended breathing while asleep. It is an important risk factor for cardiovascular disease and diabetes, so it is well worth asking patients whether they suffer breathing problems during the night and then following up those who do. More than one-third of people with sleep apnoea have hypertension, so measuring blood pressure is important in assessing risk factors and then establishing appropriate preventive treatment.
Improving the primary care management of obesity
Over half of all adults in the UK are overweight, according to latest figures. The number of people who are obese has tripled over the last 20 years, and is still rising. But is weight management an issue for primary healthcare teams? There is clear evidence that it is – with obesity being directly related to increased risk of death and a range of chronic diseases. Obesity reduces life expectancy, on average, by nine years. At long last there is some encouragement for general practices to optimise detection and management of obesity. The new General Medical Services (GMS) contract includes 208 from a total of 1050 points available in the Quality and Outcomes Framework that are affected by weight loss, offering a major financial incentive to general practices to encourage patients to lose weight.
Erectile dysfunction (ED) is a common condition that not only causes distress to a couple, but also indicates the likely presence in the man of cardiovascular and other diseases. By diagnosing and treating ED, nurses can therefore help to restore the coup
Improving the management of diabetic foot conditions
Foot complications are very common in patients with diabetes. At least one in six diabetics develop foot ulcers at some point in their lives. This article reviews why foot complications occur in diabetes, how you can detect foot problems early, and treatment and prevention strategies. The National Service Framework for Diabetes suggests that targeted foot care for people at high risk could save hundreds of amputations a year. By detecting complications earlier, we can make a real difference to patients’ lives, reducing morbidity, improving quality of life and even saving limbs.