GPs and practice nurses face many challenges when diagnosing and managing heart failure. This comprehensive supplement reviews all aspects of chronic and acute HF, from epidemiology, through diagnosis, lifestyle interventions, pharmacological and device therapies to implementation of current guidelines.
Optimising the management of heart failure
Evidence-based guidelines offer many options to improve and extend the lives of patients with heart failure (HF). This article reviews current best practice in the management of chronic HF and of acute decompensated HF, and considers recent insights, controversies and innovations in this important field.
Heart failure: Improving outcomes today
Optimising the management of heart failure improves patient survival and reduces hospital admissions. However, standards of care continue to vary, and many HF patients are still not receiving recommended therapy with disease modifying drugs or specialist input to their care. Outcomes will only improve for all HF patients if evidence-based clinical guidelines are implemented throughout the NHS.
Heart failure today: The challenge
Heart failure is an important public health problem that is associated with significant morbidity, mortality and healthcare costs, especially in the over-65s. Despite reductions in HF-related mortality, hospitalisations remain frequent and readmissions continue to rise. It is these admissions to hospital that put a financial strain on the local health economy, and cause stress and anxiety for the patient and supporting family.
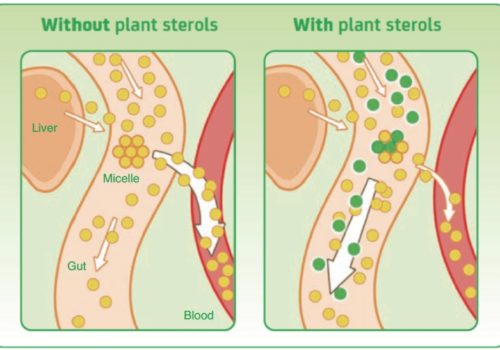
Plant sterols and cardiovascular risk
The World Health Organization recognises that 80% of CHD could be prevented by positive lifestyle changes. Healthcare professionals should encourage and support patients to quit smoking, increase physical activity, and make positive dietary and lifestyle changes to help better manage their heart health.
Briefing: Chronic kidney disease
Chronic kidney disease (CKD) is the term used to describe long-lasting abnormal kidney function and/or structure. It is common and often exists together with other conditions like cardiovascular disease (CVD) and diabetes. CKD is an essential diagnosis because treatment can reduce the risk of CVD and prevent or slow progression to kidney failure. This is your briefing on important NICE guideline changes that will help us to better identify at-risk patients while making over-diagnosis less likely.
NICE lipid modification guidelines: Statins for all?
The updated guideline on lipid modification from the National Institute for Health and Care Excellence (NICE), which was published in summer 2014, has continued to cause a great deal of controversy, both among health professionals and the general public. Now that the dust has settled just a little, it is time to review the messages of this guideline in detail rather than relying on the headlines.
Alcohol: A public health priority
Alcohol has been identified as one of Public Health England’s seven key priorities. After smoking and obesity, it is the biggest lifestyle risk factor for morbidity and mortality in the UK, accounting for 10% of disease and death. An estimated 9 million adults drink alcohol at levels detrimental to their health, with an estimated 1.6 million portraying signs of alcohol dependence. There is a misconception that drinking alcohol will only have a negative impact on health in those who binge drink or regularly get drunk. However, alcohol harms not only the individual drinker but also society as a whole, costing £21 billion a year, including annual direct costs to the NHS of £3.5 billion.
The increasing challenge of heart failure: Improving outcomes – Introduction
Despite advances in management, heart failure (HF) remains a deadly clinical syndrome, with a five-year survival of 58% compared with 93% in the matched general UK population. In this comprehensive supplement, my colleagues provide excellent reviews of all aspects of chronic and acute HF, from epidemiology, through diagnosis, lifestyle interventions, pharmacological and device therapies to implementation of current guidelines. Rather than regurgitating the content of their articles, I would like to pick out some areas worthy of thought and discussion. I will discuss challenges to clinicians in the diagnosis and management of HF, diagnostic use of natriuretic peptides (NPs), newer medical therapies and their future use, device therapies, and implementation of the evidence base into clinical practice.
The effective diagnosis of heart failure
Heart failure (HF) is a complex clinical syndrome, characterised by symptoms including breathlessness, fatigue, reduced exercise tolerance and fluid retention. Signs and symptoms may be non-specific or difficult to elicit, and some primary healthcare professionals continue to lack confidence in their ability to identify patients with HF. A systematic approach to history-taking, examination and referral aims to help improve the accuracy of the diagnosis and ensure that HF patients are referred for specialist assessment and receive evidence-based therapies.
How many more people will we need to anticoagulate using CHA2DS2VASc? A real-life study in British primary care
Managing stroke risk in people with atrial fibrillation (AF) is critical. The introduction of the CHAVASc score has lowered the threshold for consideration of anticoagulation to prevent stroke in AF. This means potentially extra work for clinicians in assessing AF patients, and an extra cost to the NHS from more medication and monitoring. This study aims to quantify the increase in the numbers of people requiring anticoagulation with the newer risk assessment score. Method: The GRASP-AF tool was used to quantify the number of people categorised as high risk, using the CHAVASc score compared with the standard CHADS score. Population: An inner-city population from nine general practices within a single Clinical Commissioning Group (CCG), covering a population of 42,274 patients. Results: A total of 395 patients were found to have AF. In this study, 64% were categorised as high risk using CHADS compared with 87% on CHAVASc. This represents an increase of 35% in the numbers of people classed at high risk of stroke and needing to be considered for anticoagulation. Conclusion: There are significant extra costs to implementing the CHAVASc score, both in drug costs and extra work for primary care, which need to be managed within the local health system. The greatest benefit will be at an individual level. Some people who would have had a stroke will be spared that experience. Who those individuals are, we will never know.
Why doesn’t telling people what to do work?
I hate being told what to do and usually I will do the opposite. So where on earth did I get the belief that I know what is right and that I must make sure I tell everyone what to do to stay healthy?