Angina is on the increase as people live longer. It is the most common symptom of ischaemic heart disease and occurs when the arteries are no longer able to supply the heart with enough blood to meet its demands. Treatment aims to restore the balance between oxygen supply and demand, to relieve the pain as quickly as possible and prevent further angina attacks, to treat the risk factors, limit the progression of coronary artery disease and reduce the risk of a heart attack. Procoralan (ivabradine) works by specifically inhibiting the If or ‘funny’ channel in the sinoatrial node of the heart (also known as the cardiac pacemaker) to reduce the resting heart rate, matching the efficacy of beta-blockers without their side-effects.
Maximising healthcare benefits for individual patients and society as a whole
Where are we now with rosiglitazone? A comment from GlaxoSmithKline
A survey of GPs’ views on clinical and cost issues in prescribing statins
Statin therapy for secondary prevention of coronary heart disease: an update
Optimising use of statins in clinical practice: how to achieve the best clinical outcomes for every patient
Procoralan (Ivabradine): A New Treatment Option for Angina
Neurolinguistic Programming: Getting to the Heart of Communication
Imagine what it would be like if you could communicate effectively with every person you meet. What would it be like to know that any messages you want to put across to your patients mean the same to them when they hear them as they mean to you? A few basic pointers in neurolinguistic programming (NLP) may help to improve how clearly you communicate with others. In this article we will look at linguistics, or the use of language, as one part of NLP and a key indicator of how people make sense of, and interpret, the world.
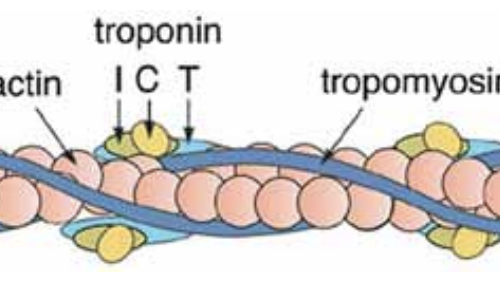
Using troponins to assess cardiac damage: Getting to the heart of the matter
Troponins are now measured routinely in patients with acute chest pain in most hospitals in the UK. Studies have confirmed that they represent a marker of risk for subsequent cardiac events in most patients. In this article we explore what troponins are, why they may increase in acute coronary syndromes, how they are measured and how likely they are to be used in the future.
Optimising Management of Supraventricular Arrhythmias
Caring for patients with arrhythmias has evolved over the past decade as a result of technological innovation in both diagnosis and treatment. This article highlights some of the most common arrhythmias and reviews the most appropriate strategies for their medical management. The National Service Framework (NSF) for Coronary Heart Disease (CHD) sets out three quality standards in the chapter on arrhythmias and sudden cardiac death and we look at how to successfully implement these.
Starting an a Beta-Blocker for your Heart Problem
Editorial
We hope this issue of BJPCN is like an Easter egg – bright and appealing on the outside, with useful articles building a solid structure that you can really get your teeth into and lots of extra chocolates inside to sustain you over the next few weeks.