Familial hypercholesterolaemia (FH) is a common monogenetic condition that causes high levels of cholesterol in the blood, resulting in an increased risk of heart disease at an early age. FH affects around one in every 270 people. That means that in England around 160,000 adults and 40,000 children under 18 years are likely to have FH, though only around 3,000 have been diagnosed by DNA testing. This article discusses the new implementation guide, which is designed to improve the identification and treatment of people with FH.
The Heart Age Test: An evidence-based, individual risk calculator
Behavioural risk factors such as poor diet, smoking and low physical activity, along with high blood pressure, high body mass index and high cholesterol are the main risk factors for cardiovascular disease (CVD). The Heart Age Test is a digital online tool designed to help make sense of an individual’s risk of CVD, the implications of that risk and the behavioural changes needed to reduce that risk.
Lipid lowering: Working with patients to take their tablets
The benefits of lipid modification therapy in reducing cardiovascular disease (CVD) risk have been well recognised since the advent of effective treatments, including the HMG-CoA reductase inhibitors (statins). Use of statins is likely to have been a contributory factor in the fall of over 75% in CVD mortality in many industrialised countries over the last 40 years. Other interventions, including improved management of other cardiovascular risk factors, notably hypertension and smoking, have also been important. However, CVD continues to be responsible for one in four premature deaths in the UK, with rates in the most deprived 10% of the population being almost twice as high as in least deprived cohorts.
Atrial fibrillation management: We can do better
Atrial fibrillation (AF) management has been transformed within the last decade by revised clinical guidance and availability of new drugs. Aspirin monotherapy, once accounting for almost half of all antithrombotic prescriptions for AF, is now an obsolete therapy. Anticoagulation is the treatment of choice for AF and direct oral anticoagulants (DOACs) have overtaken warfarin as the drug of first choice for new starters. However, management of one in four people with AF remains suboptimal, and this article reviews the major issues around antithrombotic and other treatments for AF.
Detect, protect, perfect: AHSNs going further, faster to reduce AF-related stroke
Since 2014 the 15 Academic Health Science Networks (AHSNs) across England have been working on a collaborative atrial fibrillation (AF) programme focused on reducing AF-related stroke. The national programme has three elements: Detect: finding more people with AF to allow early intervention to prevent stroke; Protect: treating more at-risk patients with anticoagulants to reduce the rate of AF-related stroke; and Perfect: improving the quality of anticoagulation to ensure maximal patient outcomes.
Pharmacist-led interventions for CVD prevention
Community pharmacists are widely recognised as an under-utilised resource within the NHS, in spite of their skills and experience, and the accessibility of their premises. In recent years, community pharmacists have demonstrated the value of the clinical services they offer, particularly in the prevention of cardiovascular disease (CVD).
‘The super intervention’ – Physical activity nurse champions
If physical activity were a pill we would prescribe it because of its wide-reaching positive impacts on major long-term conditions. The aim of this article is to outline the growing evidence base supporting the benefits of physical activity and to identify the harms from inactivity. However, only a minority of healthcare professionals seem to be familiar with the current Chief Medical Office (CMO) physical activity guidance.
Talking about sex, hormones and the heart
The NICE 2015 guidelines on the diagnosis and management of menopause provides useful evidence-based guidance on the menopause, but it is unclear if many GPs are able to confidently prescribe appropriate hormone replacement therapy (HRT). This brief article gives an overview of the importance of HRT and aims to help GPs to manage their patients experiencing menopause.
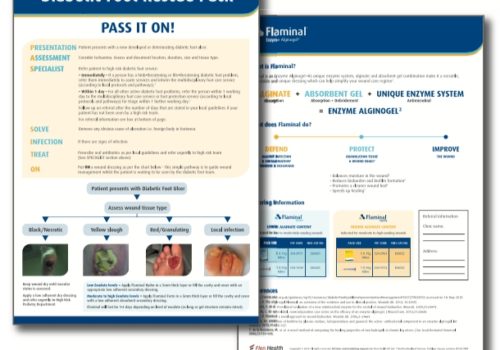
‘PASS IT ON’ – Saving legs, lives and money
Foot ulceration in people with diabetes is an increasing problem which is costly to the NHS financially and to patients in terms of quality of life. Management is complex and involves a team approach to ensure the best results for patients.
BHF blood pressure pilots: Changing the conversation about hypertension
As many as 16 million people in the UK are estimated to have hypertension, and around 7 million of these are undiagnosed. Of those diagnosed in England, one third are not receiving optimum management.
Dietary interventions for weight loss: What works?
Obesity is estimated to be responsible for more than 30,000 deaths each year, reducing lifespan by an average of nine years. The links between obesity, diabetes and cardiovascular disease are well documented, but overweight and obesity also causes 6% of cancers in the UK. These figures have resulted in warnings that obesity is the new smoking when it comes to risks to health and longevity. So the problem is clear. The challenge is to put into action what works.
CVD risk factors: New evidence, new approaches?
Cardiovascular disease (CVD) is the leading cause of death worldwide. Elevated blood pressure (BP) is the main global risk factor for premature morbidity and mortality, and the prevalence of hypertensive heart disease is not declining over time. Improved control of high BP is, therefore, fundamental to further prevention of CVD, and adoption of treatment guidelines can have a positive impact on BP-related outcomes.