Fracture liaison services (FLS) systematically target high-risk patients, offering assessment and intervention to reduce fractures. Despite official guidance, less than two thirds of local health services have established an FLS. The Crawley FLS is an example of a community-based, integrated service that has helped to reduce local hip fracture rates and save NHS costs for the local health service.
Evaluation of the Maternal Lighten Up Weight Management Service
Most overweight/obese pregnant women gain more weight than they should during pregnancy, which can lead to adverse maternal and neonatal outcomes. This study evaluated the Maternal Lighten Up service, in which obese pregnant women are referred by their midwives to a choice of several weight-management programmes. Weight is measured at the start and self-reported at the end of pregnancy. Of women referred, only 36% started a programme. The Health Trainers programme was most popular and most frequently attended, followed by Slimming World. Participants attending Slimming World and dietetic programmes were less likely to exceed Institute of Medicine guidance on weight gain during pregnancy, but these data are based on low follow-up rates of weight at the end of pregnancy. This study provides insight into the preferences and behaviour of obese pregnant women referred to different weight management programmes, and the findings may contribute towards shaping future maternal obesity weight management services.
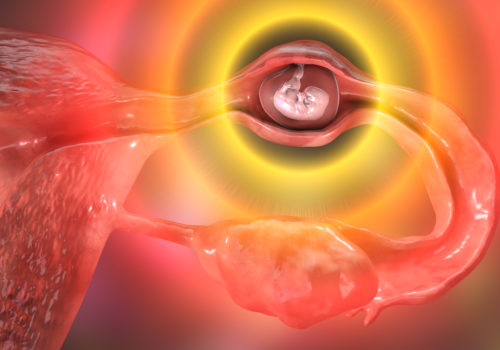
Early pregnancy loss: can we improve our practice?
The majority of pregnancies progress successfully, but some result in a miscarriage or in an ectopic pregnancy. About two-thirds of the related maternal deaths are associated with substandard care due to late or missed diagnosis. Recent NICE guidelines aim to improve outcomes for women, and this article provides practical information on how the new recommendations impact on day-to-day practice in primary care.
Contraception and sexual health for young people
Young people under the age of 18 present particular challenges for many health professionals, and a structured approach is essential when providing services for this age group. Health professionals have a responsibility to provide information in an approachable manner on all methods of contraception, including long-acting reversible contraception (LARC), and the prevention and testing of sexually transmitted infections (STIs). Professionals also need to be able to accurately assess a young person and undertake safeguarding as needed.
Subfertility: time is of the essence
More couples are now starting their families later in life, a social trend that coincides with a rise in the number of people requesting referral for treatment of subfertility. In response, the National Institute for Health and Care Excellence (NICE) has updated its fertility guidelines to enable more patients to receive timely, appropriate and successful treatment.
Lung cancer: A rising risk for women
In the UK, more women die from lung cancer than any other cancer, including breast cancer. Smoking is by far the commonest cause, and lung cancer rates are continuing to rise in women who started to smoke in the 1960s. It is never too late for anyone to give up smoking, even after a diagnosis with lung cancer, when early intervention may result in cure or significantly prolong life.
Supporting women with genital herpes
Genital herpes is a common sexually transmitted infection, especially among young adults. It may be associated with complications, notably in pregnant women, but it is not usually life-threatening. However, the diagnosis continues to attract stigma, and patients need reassurance and support as well as effective treatment.
Connecting for Women’s Healthcare
One of the great by-products emerging from the Primary Care Women’s Health Forum (PCWHF) is connectivity. Our members are becoming more aware of local initiatives in other parts of the country, and are connecting with and learning from other clinicians to share best practice in women’s healthcare.
Take a new approach to premenstrual disorders
Premenstrual disorders (PMD) are common and have a major impact on the lives of women. Until recently there has been confusion around definitions, leading to difficulties in diagnosis and management. This article describes a new consensus definition and diagnostic criteria for PMD, and advises on the choice of evidence-based treatment.
Made to measure: Tailoring oral contraception to each woman
Individualising choice of oral contraception to each woman is important to ensure safety, and enhance patient acceptability and adherence. However, tailoring should extend beyond simply deciding whether to use a combined or progestogen-only pill. Prescribers should also bear in mind the non-contraceptive benefits of each product, and consider alternative regimens for women with hormone-related medical conditions or those who wish to avoid menstrual bleeds.
Fertility problems
If you have fertility problems, it means you have difficulty in conceiving (becoming pregnant) despite having regular sex without using contraception. Before you begin to worry, remember that many couples take several months to conceive. Over eight in 10 couples conceive within a year of trying, while about nine in 10 conceive within two years.
Practical prescribing to promote urinary continence
Urinary incontinence and related conditions have a high prevalence and a major impact on a patient’s quality of life. Drug therapy can be very effective and forms an important part of the treatment armoury when managing women with incontinence. Unfortunately, medication can be associated with adverse effects, but there are approaches that can be used to maximise a drug’s effectiveness and limit problems that reduce adherence to treatment.